 |
Low carb, or fat? Left or right? Which one should you chose and why? Shall you go by your body weight, your insulin sensitivity or your personal food preferences? |
You can learn more about improving your body composition at the SuppVersity
 |
| Figure 1: Weight loss (kg) after 6 months on the respective in insulin resistant and sensitive subjects (Gardner. 2015). |
 |
| Figure 2: Proportions of carbohydrates, fats, and proteins for each diet at baseline, 3 months, and 6 months (Gardner. 2015). |
Limbo-Titrate-Quality: The dietary strategy that was used is quite interesting and actually something worth copying for yourself or your clients. There was the "Limbo" phase where the fat or carb intake had to be cut back drastically to 20 g/day of total fat or digestible carbohydrates. The goal of this phase was, as the scientists point out "to achieve the lowest level of fat or carbohydrate intake within the first 8 weeks" (Gardner. 2015). In the second stage, the scientists labeled as the "Titrate" phase the subjects slowly added fat or carbohydrate back to their diet - in increments of 5 g/day (e.g., from 20 to 25 g/day). With each increase, the intake had to be maintained stable for at least 1, maximally 5 weeks before adding another 5 g/day. The (good) idea was to allow each of the participants (in what the researchers call stage 3 of the intervention, although 2 + 3 appear to depend on each other) to find his or her specific level of fat or carbohydrate intake he / sheh "could be maintained long term, potentially for the rest of their lives" (ibid). The fourth and last stage eventually focused on diet quality. In the "Quality" phase the subjects had to maximize the nutrient density of their foods by selecting whole foods, buying organic, grass-fed, etc.
As you can see significant inter-group differences were observed only for the macronutrient composition; and even though these differences were significant, we are nor talking about a ketogenic vs. no-fat diet. Rather than that, both diets had a relatively balanced macronutrient profile, albeit with different main energy sources (carbs vs. fat). What did not differ for the groups, though was the total energy intake (Figure 2). This is interesting, because, in theory, the subjects were allowed ot eat as much as they wanted; and still, the data in Figure 2 tells you that they restricted their energy intake by noteworthy 30% on average (the ~600kcal-deficit also explains why the subjects even lost weight), with no difference between the subjects on the allegedly more satiating low carb vs. low fat diet.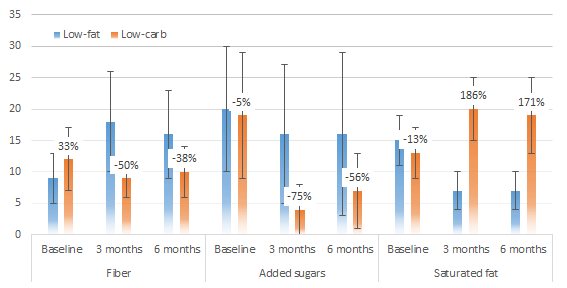 |
| Figure 3: Fiber, added sugar and saturated fat intake in g/1000kcal (Gardner. 2015). |
So, what's healthier, then? Low carb or low fat? To answer this question, researchers from the University of Oslo have recently conducted a meta-analysis that yielded quite interesting results, when the individual findings from the studies were pooled as weighted mean difference (WMD) using a random effect model: Compared with participants on LF diets, participants on LC diets experienced a greater reduction in body weight (WMD –2·17 kg; 95 % CI –3·36, –0·99) and triglicerides (WMD –0·26 mmol/l; 95 % CI –0·37, –0·15), as well as a greater increase in HDL-cholesterol (WMD 0·14 mmol/l; 95 % CI 0·09, 0·19) - that's good. Unfortunately, they also saw signficant increases in LDL-cholesterol. With 0·16 mmol/l, the mean difference in LDL was larger than the mean HDL increase, which could suggest an increase in CVD risk and has the authors conclude that their "findings suggest that the beneficial changes of LC diets must be weighed against the possible detrimental effects of increased LDL-cholesterol" (Mansoor. 2015). Personally, I would say, though, that for the mostly obese subjects in the studies, the weight loss and reduction in triglycerides (likewise a marker of CVD risk) are more important than the increase in LDL-C - future studies should try to elucidate if the particle size and LDL oxidation worsened as well and what the actual long-term (years, not months) effects are.
It is thus no wonder that the data from blood analysis of the study at hand (Figure 4) mirrors the results of the studies Mansoor et al. (2015) analyzed for their meta-analysis that is about to be published in the British Journal of Nutrition (see red box): |
| Figure 4: Changes in LDL-C, HDL-C, Trigs and fasting glucose after 3 & 6 months (Gardner. 2015). |
This doesn't solve the dilemma we're in, though: without further data on particle sizes and oxidative status of the LDL molecules, etc. it is virtually impossible to make a reliable prediction which of the two diets is going to have the higher long-term health benefits. What may be even more important, though, is that we must not forget that it is not debatable that both diets triggered significant weight loss and measurable health improvements, especially in the subjects with pre-existing insulin resistance (blue and orange bars in Figure 4).
 |
| Figure 5: Changes in the prevalence of metabolic syndrome after 3 and 6 months (Gardner. 2015). |
The significant intra-group differences, however, tell us that whether you are or aren't insulin resistant is not the only determinant of your response to the different diets. Especially for healthy individuals experimentation and finding what suits you, your lifestyle and sports best does therefore still appear to be the way to go.
In those with pre-existing metabolic syndrome (which is more than just insulin resistance, by the way), the generally higher relative reduction in MetSyn prevalence Gardner et al. observed in their study (Figure 5) do yet appear to confirm the general trend towards low-carbohydrate diets for people with serious metabolic issue; and maybe that's actually the main take-home message of a study that must be seen as a first attempt to identify one of the variables that determine whether an individual thrives on a low carb, a low fat or maybe just a completely balanced diet | Comment!
- Gardner, et al. "Weight Loss on Low-Fat vs. Low-Carbohydrate Diets by Insulin Resistance Status Among Overweight Adults and Adults with Obesity: A Randomized Pilot Trial" Obesity (2015): Ahead of print.
- Mansoor, et al. "Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials." British Journal of Nutrition (2015): First view article.




