 |
| Now you tell me there was nothing magic about milk (poster from the CMPB "Got Milk" campaign) |
Hey, David! Is there something magic about milk?
I would also like to emphasize that both explanations I presented to explain the absence of beneficial effects of full-fat dairy and the non-significant detrimental effects of full-fat milk, yesterday, are just as the word implies "hypothetical" and I am not claiming to be sure that any of them fully explains the high vs. low fat difference. To be honest, I would be flabbergast if only one of them was the - meaning the only - reason that full-fat milk consumption does not yield the same reductions in diabetes risk as skim or low fat milk (and dairy in general).
Even the common notion that a high omega-6 to omega-3 ratio could be the culprit (hypothesis II, in yesterday's show), is by no means non-debatable; and that despite the fact that the current vilification of omega-6 fatty acids as yet another "root of all nutritional evil" would suggest so:
- A 2012 study from the Uppsala University, for example, found in a one-to-one comparison of a high linoleic acid (omega-6) vs. saturated fat (SFA) diet that those of the 61 abdominally obese subjects (15% had type 2 diabetes) who had been assigned to the diet that was high in vegetable n−6 PUFA instead of the SFA diet (butter), had much better fasting insulin levels (64.2pmol/L vs. 79.0 pmol/L), recorded a small but significant positive effect on the visceral / subcutaneous adipose tissue ratio and even reduced their body fat percentage minimally (-0.1% vs- +0.6% in the "buttered" group; cf. Bjermo. 2012). Surprising if you stick to the mainstream all-across the board condemnation of cones (baked-on sunflower oil), margarine, sunflower oil, and sunflower seeds, which were the main dietary PUFA sources in the high PUFA group, isn't it?
- On the other hand, mechanistic insights into the underlying cause of the detrimental effects of the saturated fat can be found, among others, in Lee et al. (2006) who report that the diaglycerol build-up (DAG) in skeletal muscle that occurs when you feed rodents a high saturated fat diet is responsible for the subsequent development of insulin resistance that was observed by Bjermo et al. in their previously cited human study (Lee. 2006)
Here is a simply truth: Your milk contains, what your dairy cows eat
With the emerging evidence on the overall health benefits of a low(er) n6:n3 ratio it is still important to be aware that the n-6:n-3 ratios do vary significantly even for those cows that would be considered "pasture fed" depending on the actual amount of pasture in their feed (5:1 for 1/3 pasture, 1.9:1 for 2/3 pasture and 0.7:1 for all pasture; cf. Dhiman. 1999; figure 2, left).
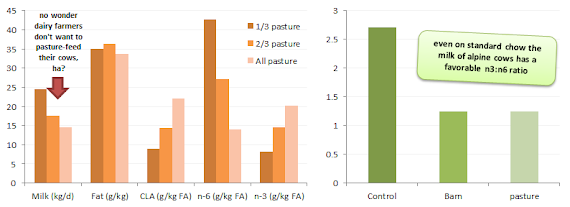 |
| Figure 1: Milk fatty acid composition depending on amount of pasture in the diet (left, Dhiman. 1999); n-6:n-3 ratio of milk from alpine cows depending on the feed they received (right; Leiber. 2005) |
So if it's not the omega-6 content reduces the value of full-fat milk?
Obviously, these insights leave us with the question what else it may be that links regular full-fat milk and diabetes. Also: Why is this link not significant? In the end, it could simply be adding full-fat milk on a diet that already has plenty of fat and sugar in it that's the problem - not all people who consume high amounts of milk would yet fall into this category so that you would see those with an otherwise spot on diet benefit, while those on the standard American diet are doing more harm than good. If we also consider the real-world bias due to the bad rep of full-fat and good reputation of skim or low fat dairy, it should be obvious that your average low fat dairy eater is more likely to watch his diet than his high fat dairy loving neighbor. Together this could certainly explain why the results suggest a statistically non-significant 12% risk increase per 200g of full-fat dairy per day - the gap between those who benefit and those harm themselves is simply too wide to achieve statistical significance.
read more). You could for example argue that you will either consume homogenized or non-homogenized full-fat milk, but won't jump back and forth between the two because one (the homogenized milk) does not even taste like milk (and this is not just my opinion ;-) - if the homogenization hypothesis which does not necessarily say that homogenization is bad, but that it will reduce the beneficial effects of the larger sized lipids (cf. Oosting. 2013; learn more) that are broken down when the milk is forced at high pressures through a <1 µm sieve.
What about estrogens in milk?
And what about cancer? The evidence that milk induces cancer is at best weak (Chagas. 2012). Even from a mechanistic point of view, dairy can only promote cancerous growth by its general growth promoting effects (those are exerted via the IGF, mTOR, Akt pathway, by the way; the same pathway that makes your muscles grow, as well). Moreover, there is evidence that dairy reduces the incidence of cancer in the digestive tract (-16% in men; -23% in women; cf. Park. 2009); and as far as prostate and breast cancer risk is concerned, there is significant evidence almost exclusively for high fat milk and (when measured) always in the presence of evaluated IGF-1 levels.
While a recent follow-up of the Nurses' Health Study (yeah, yet another one; and, yes! I am fed up with it, too) claims that the already minimal association of dairy consumption with a later transition into menopause (~3months on average) could be to the "hormonally active nature" (Carwile. 2013) of milk, it is pretty certain that this is not a result of it's estradiol content, because...So, the bottom line here is simple: A high dairy consumption within a high energy diet + chronic inflammation context will certainly boost cancer growth more than a generally growth-retarding vegan diet - that's for sure! This does yet not mean that "dairy causes cancer".
- ...the effect was observed only for low fat dairy and low fat milk, which has a much lower estradiol content than the full-fat varieties that did not postpone the onset of menopause
- ...even the highest estrogen (and highest fat, by the way) common dairy product, namely butter, has an E2 content of "only" 82pg/g (Wolford. 1979), so assuming you were eating a whole 250g packet of butter everyday you would get a pretty whopping amount of 20,500pg of E2 from it, but even if you extracted that and injected it right into your bloodstream you would end up with "only" ~4.1pg/ml in your blood and that's way below the lower limit for men which is 14pg/ml and almost 100x below the preovulatory peak value in women.
So, if milk does have any "hormonal" side effects those are probably mediated, but not necessarily caused by it's indirect effect on IGF-1 production (see box on the right).
Everything in moderation and statins only when they are really necessary: Before I wrap things, up I want to briefly mention the active ingredients of the pro-obesogenic statins, which are Rosuvastatin (Crestor; causes NAFLD, as well), Atorvastatin (Lipitor), Fluvastatin (Lescol, Canef, Vastin), Lovastatin (remember: we are talking about subcutaneous fat which is rarely measured in pertaining studies and may thus hitherto been overlooked). And let's not forget an "honorable mention": Simvastatin (Vitoryn & Inegy) was the only statin in the study from the University of Pais Vasco (Aguirre. 2013) that did not lead to a further deterioration of the already compromised insulin sensitivity of the obese rodents.
And what about humans? The increase in diabetes risk is real. Not just in rodents. The increased diabetes risk due to statin treatment Satar et al. calculated in their 2010 meta analysis of 13 trials with more than 90,000 subjects is ~9%. If you want to learn more about the study, click here to watch a video interview with Prof. Satar. He also elaborates why patients at high risk of heart disease (which is not everyone with high cholesterol) can still benefit from statin treatment and how muscular side effects and effects on the liver could be the underyling cause of the increase in diabetes risk he and his colleagues observed.
 |
| Suggested read: "Ask Dr. Andro: Are Colostrum and Milk Products in General Healthy Muscle Builders, a Waste of Money or Toxic Waste?" | read more |
In a very similar vein, consuming a gallon of low fat dairy is NOT going to reduce your diabetes risk to zero (although basic math may suggest that) - everything in moderation, folks ;-)
References:
- Aguirre L, Hijona E, Macarulla MT, Gracia A, Larrechi I, Bujanda L, Hijona L, Portillo MP. Several statins increase body and liver fat accumulation in a model of metabolic syndrome. J Physiol Pharmacol. 2013 Jun;64(3):281-8.
- Aune D, Norat T, Romundstad P, Vatten LJ. Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am J Clin Nutr. 2013 Aug 14. [Epub ahead of print]
- Bjermo H, Iggman D, Kullberg J, Dahlman I, Johansson L, Persson L, Berglund J, Pulkki K, Basu S, Uusitupa M, Rudling M, Arner P, Cederholm T, Ahlström H, Risérus U. Effects of n-6 PUFAs compared with SFAs on liver fat, lipoproteins, and inflammation in abdominal obesity: a randomized controlled trial. Am J Clin Nutr. 2012 May;95(5):1003-12.
- Carwile JL, Willett WC, Michels KB. Consumption of Low-Fat Dairy Products May Delay Natural Menopause. J Nutr. 2013 Aug 14. [Epub ahead of print]
- Chagas CE, Rogero MM, Martini LA. Evaluating the links between intake of milk/dairy products and cancer. Nutr Rev. 2012 May;70(5):294-300.
- Dhiman TR, Anand GR, Satter LD, Pariza MW. Conjugated linoleic acid content of milk from cows fed different diets. J Dairy Sci. 1999 Oct;82(10):2146-56.
- Fotherby K. Bioavailability of orally administered sex steroids used in oral contraception and hormone replacement therapy. Contraception. 1996 Aug;54(2):59-69. Review.
- Lee JS, Pinnamaneni SK, Eo SJ, Cho IH, Pyo JH, Kim CK, Sinclair AJ, Febbraio MA, Watt MJ. Saturated, but not n-6 polyunsaturated, fatty acids induce insulin resistance: role of intramuscular accumulation of lipid metabolites. J Appl Physiol. 2006 May;100(5):1467-74.
- Leiber F, Kreuzer M, Nigg D, Wettstein HR, Scheeder MR. A study on the causes for the elevated n-3 fatty acids in cows' milk of alpine origin. Lipids. 2005 Feb;40(2):191-202.
- Mansbridge RJ, Blake JS. Nutritional factors affecting the fatty acid composition of bovine milk. Br J Nutr. 1997 Jul;78 Suppl 1:S37-47.
- Oosting A, van Vlies N, Kegler D, Schipper L, Abrahamse-Berkeveld M, Ringler S, Verkade HJ, van der Beek EM. Effect of dietary lipid structure in early postnatal life on mouse adipose tissue development and function in adulthood. Br J Nutr. 2013 Jul 11:1-12. [Epub ahead of print]
- Park Y, Leitzmann MF, Subar AF, Hollenbeck A, Schatzkin A. Dairy Food, Calcium, and Risk of Cancer in the NIH-AARP Diet and Health Study. Arch Intern Med. 2009;169(4):391-401.
- Sattar N, Preiss D, Murray HM, Welsh P, Buckley BM, de Craen AJ, Seshasai SR, McMurray JJ, Freeman DJ, Jukema JW, Macfarlane PW, Packard CJ, Stott DJ, Westendorp RG, Shepherd J, Davis BR, Pressel SL, Marchioli R, Marfisi RM, Maggioni AP, Tavazzi L, Tognoni G, Kjekshus J, Pedersen TR, Cook TJ, Gotto AM, Clearfield MB, Downs JR, Nakamura H, Ohashi Y, Mizuno K, Ray KK, Ford I. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet. 2010 Feb 27;375(9716):735-42.
- Simopoulos AP. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed Pharmacother. 2002 Oct;56(8):365-79.
- Wolford ST, Argoudelis CJ. Measurement of estrogens in cow's milk, human milk, and dairy products. J Dairy Sci. 1979 Sep;62(9):1458-63.
