 |
| Macronutrient ratios matters, but food quality does, too. And so do exercise, laziness, sleep, .... the list is endless, so can we be surprised that modulating GI and protein is not helping much? |
In view of the fact that you're still there, I suppose that I was wrong and you are interested in the effects of different marconutrient ratios and types of carbohydrates (low vs. high glycemic index) on weight loss and glucose management. Let's take a closer look at the design of the DiogenesTrial (learn more), then.
Use alternatives to sugar sweetened beverages if you want to improve your blood glucose!
- The intended difference in protein content of the LP and HP diets was 10%–12% of energy intake.
- The intended difference in glycemic index between the LGI and HGI diets was 15.
 |
| Table 1: Examplary diet composition in the Diogenes Trial (van Baak. 2014) |
Lifestyle changes are more powerful than supplements: So don't forget that it's imperative to realize the lifestyle changes described in the first installment of the "Improve Your Glucose Sensitivity"-series. Otherwise the best you can hope to achieve with supplements (and drugs) is to slow the progression from insulin resistance to full-blown diabetes.
The analysis of the three-day dietary records showed the expected differences in carbohydrate content and glycemic index between the diet groups, but the differences were smaller than intended (a bummer in view of the fact that they were not large to begin with). Much in contrast to what our initially phrased prejudice would say, there were no significant differences in mean 24-h, daytime or nighttime glucose concentrations between the diet groups.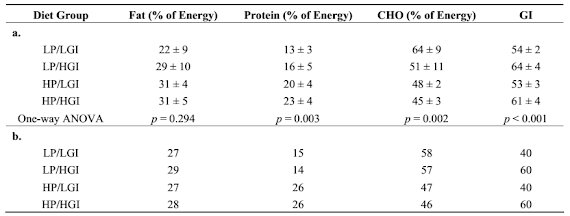 |
| Table 2: Self-reported dietary macronutrient composition in the field study (a) and macronutrient composition of the diet in the lab study (b) (van Baak. 2014) |
"Post hoctesting did not reveal differences between the LP/HGI diet and any of the other diets for the glucose parameters studied. Adjustment for BMI, HOMA-IR (Homeostatic Model Assessment of Insulin Resistance) index, minutes of exercise performed by the subjects, total weight loss or weight regain did not change this outcome (data not shown)." (Van Baak. 2014)Still, in a relatively uncontrolled scenario like the one in the Diogenes Study it's always possible that someone cheated twice, i.e. he deviated from the diet and reported to have stuck to it to the literal "T". Against that background, the results of van Baak's three-day follow up in a very controlled scenario is all-the-more interesting.
 |
| Figure 1: Parameters of glucose homeostasis means (left) and standard deviations (right) on the different diets in the lab study (van Baak. 2014) |
To find an effect that is statistical significant we do thus have to take a look at the continuous overlapping net glycemic action over 1 h periods (CONGA1) values over 24 h on the different diets in the lab study, where the high protein + low GI group finally shows the statistically significant advantage we've been waiting for all along (see Figure 2). Still, as the scientists point out, overall their data does not support the hypothesis that "glucose concentrations would be highest on the reference diet (LP/HGI) compared to all other diets and especially compared to the HP/LGI diet." (van Baak. 2014). As the author points out, the study did yet provide support for the hypothesis regarding glucose variability was found, since both 24-h and daytime variability of glucose concentrations were lower on the HP/LGI diet than on the LP/HGI diet.
 |
| Learn how to improve and maintain your insulin sensitivity in a previous article and the corresponding series about ways to improve your insulin sensitivity, naturally. |
That being said, there is no doubt that a high(er) protein, low(er) GI will make it much easier to return to the realms of the few non-pre-diabetics. In that, the effects will probably be even more profound if you increase the protein intake by more than 10% over the reference value of 0.8g/kg.
Doubling the protein intake, for example, would necessarily require a reduction in carbohydrate and fat intake of 3.2kcal/body weight. For a person who weighs 100kg that would be 320kcal and 80g of carbs or 40g of fat - with the former usually being the better idea for anyone who's still significantly overweight and not already eating less than 180g of carbs per day.
- van Baak, Marleen. "24-Hour Glucose Profiles on Diets Varying in Protein Content and Glycemic Index." Nutrients 6 (2014):3050-3061



