![]() |
| Some say "fat is a mistake" others say "it was our fattest mistake to believe just that" - who is right? Or are things eventually more complicated than that? |
In the
last installment of this
series, we've covered the relatively well-known, but rarely well-understood beneficial effects of protein on glucose homeostasis in humans (⤷
go back and read it).
This week we will make a fat transition (all puns intended) to the 2nd macronutrient that exerts non-carbohydrate dependent effects on glucose homeostasis: FAT!
We have known for decades that the acute glycemic response is affected by the fat content of the diet.
As my German "friends", Martina Heer and Sarah Egert, whose recent paper in the scientific journal
Diabetes/Metabolism Research and Reviews inspired me to write this article series point out, a recent meta-analysis of the existing literature on low-carbohydrate + high-fat diets suggests that these diets, unlike high-carbohydrate and high glycemic index diets, may be effective in improving glycemic control, weight, and lipid profiles (Schwingshackl. 2011).
You can learn more about this topic at the SuppVersity ![]()
Proteins, Peptides & Blood Glucose
![]()
SFA, MUFA, PUFA & Blood Glucose
![]()
Read these ➲ while waiting
![]()
Low Fat Advantage on IF
![]()
16 Weeks High Fat Diet
![]()
Fat to Blunt Insulin?
In view of the fact that I may probably safely assume that you haven't been living under a rock for the past 10 years, I would be impressed if you consider the results Schwingshackl et al. presented in the
Annals of Nutrition and Metabolism news.
We all know that there is hardly a better way to reduce blood glucose levels than not eating carbohydrates, but if you look at the title of this series and my goal to present an analysis of the effects of
non-carbohydrate nutrients on blood glucose homeastasis in humans, it should be obvious that
low carb diets must be excluded from this overview. What we will focus on in this installment is thus
- the general effect of dietary fat on the absorption, appearance and clearance of glucose from the bloodstream, and
- the different effects of saturated, monounsaturated, and polyunsaturated short- and long-chain fatty acids on glucose homeostasis
Now that you all know our plan of attack, let's get right straight to the facts and our close analysis of the contemporarily available data. There is a myriad of different fatty acids in our diets, but we don't even understand the role of the most abundant ones, which are oleic acid, linoleic acid, palmitic acid, and stearic acid completely.
Where are the short chains? If you are honest, this is an unwarranted question. We are, after all talking about "non-carbohydrate nurtients" from your diet, here and last time I checked, the production of short chain fatty acids in our guts required dietary carbohydrates. If we discard the 3-4% of butyrate quality butter, you will thus have to consume resistant starches to benefit from the proven anti-diabetic, anti-obesity effects that is brought about by the interaction of gut derived short chain fatty acids with "their" receptor, ie. GPR43 (den Besten. 2013; Kimura. 2013).
The ratio of these monounsaturated, polyunsaturated and saturated fatty acids in our diet determines our own molecular built, meaning: The dietary acid composition of our diet has both acute mechanistic, and chronic structural effects on our cells, which are mediated by the storage of fatty acids in tissues and cell membranes (Carlson. 1986).
![]() |
| 27nmol/L LDL Per 1% Reduction in Trans Fat Intake | learn more |
A high intake of trans-fats for example will lead to an accumulation of trans-isomers of linoleic acid in the heart and a highly significant 50% risk increase for cardiac arrest (Lemaitre. 2002).- A high concentration of linoleic acid (n-6) in the erythrocyte membrane has been shown to be negatively, a high palmitic acid content positively associated with incident type 2 diabetes in 1346 Finnish men aged 45–73y researchers from the University of Eastern Finland followed for 5-years in recently conducted a population-based study (note: The researchers detected no protective effect of omega-3 fats; cf. Mahendran. 2014).
I could easily extend this list, but I assume that you're getting the idea of the significant interactions between the fatty acid composition of cell membranes and the various functions and attributes of the cells (eg. membrane fluidity, ion permeability, and insulin receptor binding or affinity), which can affect both, local as well as systemic insulin sensitivity.
![]() |
| Fatty acid ⇆ PPAR interaction (Kota. 2005) |
"More recent experimental data also point toward other mechanisms which involve direct regulatory effects on gene expression and enzyme activity.
For example, in vitro studies and studies in animal models suggest that fatty acids could act directly on insulin-sensitive tissues (Risérus. 2008)." (Heer. 2014)
In the six years that have passed since the overview by Risérus et al. (2008) Heer and Egert cite in their paper has been published, we have learned much about these direct effects. You all know the effects fish oil, conjugated linoleic acid and co have on the peroxisome proliferator-activated receptors (PPARs) and the corresponding downstream effects on glucose uptake and the storage of superfluous energy in the adipose organ (Kota. 2005. Grygiel-Górniak. 2014).
PUFAs, PPARs and the key to becoming a healthy obese individualAccording to the most recent review of the literature, the PPAR-gamma receptor which is activated primarily by unsaturated fatty acid and their metabolites (15- hydroxy eicosatetraenoic acid, 9- and 13- hydroxy octadecadienoic acid, 15-deoxy 12,14-prostaglandin J2, and prostaglandin PGJ2), is the master regulator of glucose homeostasis and lipid storage. Against that background it is no wonder that Risérus concludes his previously cited review on the note:
"Substituting saturated fat with unsaturated fat seems to have beneficial effects on insulin sensitivity, although the clinical significance of modifying fat quality alone is still unclear." (Risérus. 2008)
It's after all an increase in insulin sensitivity that is - at least in the chronic overfeeding scenario, we call the "standard American diet" - an increase in insulin sensitivity that is paid for with increased adiposity - a phenomenon that's related to the pro-adipogenic effects of PPAR-gamma and one that diminishes the usefulness of thiazolidinediones like
pioglitazone, which are mostly pan(=all) agonists of the peroxisome proliferator-activated receptors, in the battle against diabetes. At least, if you share my opinion and think that treating an already overweight diabetic with a drug that will lead to significant weight gain (Khan. 2002) could do more harm than good in the long run.
The fact that the anti-diabetes effects of PUFAs are mediated by their adipogenic effects does not mean that you have the choice between pest and cholera, but the PUFA induced increase in insulin will always be a double-edged sword, as long as you are consuming significantly more energy than you're expending.
Still, if our main concern is blood glucose management in an overfeeding scenario (=the Western real word), the international recommendations to reduce the intake of saturated fatty acids (SFA) to ≤10% of total energy intake (Aranceta. 2012) do appear warranted. And if replacing them with carbohydrates is not an option, because (a) we are talking about the influence of non-carbohydrate nutrients and (b) "[n]o clear association between SFA intake relative to refined carbohydrates and the risk of insulin resistance and diabetes has been shown" (Astrup. 2011), we will probably have to resort to protein (see
last installment) or mono- and polyunsaturated fatty acids. Both have been shown to exert beneficial effects on glucose and lipid homeostasis, as well as other important health markers.
MUFAs boost resting energy expenditure: Next to its beneficial effects on blood glucose and lipid management, a high intake of monounsaturated fatty acids can also increase the resting energy expenditure in humans by 3% in the fed and 4% in the fasted state, respectively (Kien. 2013).
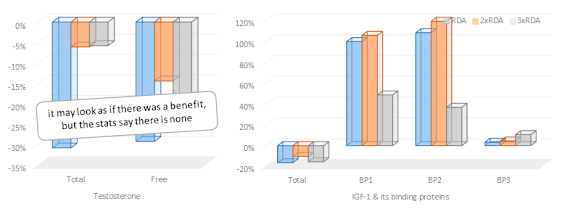
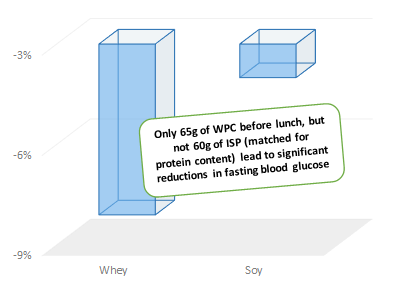
Monounsaturated fats - MUFAs -- Gadgil et al. report that 2 weeks on high MUFA diets lead to prompt improvements in insulin sensitivity in 64 individuals with prehypertension or stage 1 hypertension without diabetes (Gadgil. 2013). Two years before Gillinghan et al. wrote in a review of the effect of high mono-unsatuarated fatty acid intakes that the "[c]onsumption of dietary MUFA promotes healthy blood lipid profiles, mediates blood pressure, improves insulin sensitivity and regulates glucose levels" (Gillingham. 2011). - Polyunsaturated fats = PUFAs -- Similar beneficial effect on heart health have been reported for the replacement of saturated fat with polyunsaturated fatty acids (both, omega-3 and omega-6; see Flock. 2014). Evidence for the beneficial effects of omega-3 fatty acids, in particular, dates back to the late 1980s, when Popp-Snijders et al. observed that 8 weeks of daily supplementation of 3 g of the omega 3 fatty acids eicosapentaenoic and docosahexaenoic acid improves the insulin sensitivity of subjects with non-insulin-dependent diabetes (Popp-Snijders. 1987).
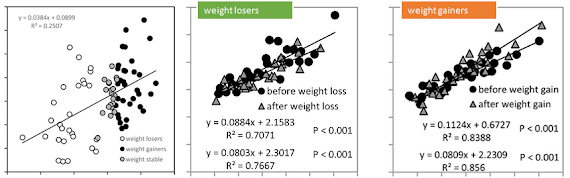
Unfortunately, studies like this have triggered an unwarranted euphoria even among healthy individuals, whose hope for further improvements in insulin sensitivity are not just unwarranted (Risérus. 2008), but could actually mislead them to mimic the high-dose fish oil supplementation regimen of the diabetic subjects in a 2006 study by Mostad et al. (1.8 g 20:5n−3, 3.0 g 22:6n−3, and 5.9 g total n−3 fatty acids from fish oil) to end up with a similar negative effect on blood glucose levels and glucose utilization (see Figure 1). ![]() |
| Figure 1: Blood glucose levels (left), glucose utilization and C-peptide levels (right) of 26 diabetic subjects after 8 weeks of high dose fish oil vs. corn oil supplementation (Mostad. 2006) |
It must be said, though, that the Mostad study is an exception. Most fish oil supplementation studies used lower amounts of fish oil and showed improvements in lipid metabolism, but no effect on insulin sensitivity, similar to those Kabir et al. observed in 2007. Accordingly, reviewers agree fish oil supplementation in moderate dosages (equivalent to 1-2 g/day n-3 LCPUFA) has no significant adverse effects on fasting glucose, HbA1c, fasting insulin, or insulin sensitivity (McManus. 1996; Friedberg. 1998; Montori. 2000; Lombardo. 2006; Akinkuolie. 2011; Lee. 2013) - unfortunately, it does not improve these parameters, either.
If we take a look at the null-results (=no difference in insulin sensitivity between groups) Lovejoy et al. present in their 2002 study on the effects of "high" MUFA, SFA and trans-fatty acid diets with only 9% of the total energy being based on the corresponding fatty acids, it is yet questionable how "high" the saturated fat intake has to be to elicit negative effects (Lovejoy. 2002).
Are transfats fat burners? It is certainly counter-intuitive, but in the Lovejoy study, the 9% transfat (elaidic acid) diet did not leave the insulin sensitivity of the 25 healthy men and women who participated in the trial unchanged, they did also increase the oxidation of fatty acids by 21% compared to the high MUFA diet (Lovejoy. 2002).
If we compare the results of the Lovejoy study to those Vesby et al. present in their 2001 paper, it would appear that the perviously cited 10% of the total energy intake
could actually be a realistic upper intake level. With 17% of the total energy the diet in Vesby's 3 months study had a significantly higher saturated fat content - high enough to produce a -10% reduction in insulin sensitivity compared to baseline (-12% compared to high MUFA control). Similar negative effects have been observed in the Rosquist (2014) study, I wrote about only a couple of days ago (see "Saturated Fat Makes You Fat!" |
read more).
This wouldn't be the
SuppVersity, though, if I didn't list at least two of the "on the other hands" we haven't discussed yet. Firstly, there are no long-term dietary intervention studies that would support the results of these and other 4-12 week interventions.
Is palmitic acid the bad guy? If SFAs impair insulin action, are all SFAs equally bad? Possibly not, but there is still insufficient evidence to prove this. Vessby et al. proposed that especially high proportions of palmitic acid may promote insulin resistance, and that a major role of SCD-1 may be to reduce the availability of palmitic acid in body tissues by converting it to palmitoleic acid. And while it appears as if palmitic acid had most significant negative effects on cellular glucose transport, fat oxidation, ceramide synthesis, cellular signalling, apoptosis and lipogenesis, conclusive evidence that "it's just palmitic acid that's the problem", is still missing.
And secondly, and probably more importantly, none of the studies investigated the interactions between the saturated fat and carbohydrate content of the diets. As I pointed out right at the beginning of this article, there is little doubt that a high fat diet with a minimal carbohydrate content
will lower the average blood glucose levels of (pre-)diabetic individuals - in this case, the negative effects of palmitic acid on the insulin sensitivity of skeletal muscle (Sawada. 2012), fat cells (Kennedy. 2009), and the hypothalamus (Benoit. 2011) are irrelevant, anyway. No carbs, no increase in blood glucose, no need for insulin stimulated glucose uptake... ah, and not a topic for this article series, since it is about the influence of "non-carbohydrate" nutrients on blood glucose levels.
Another of these non-carbohydrate nutrients that got an honorable mention as purported fat burner in a couple of paragraphs before are cis- and transfats. Isomeric fatty acids with the same number of carbon and hydrogen atoms, but very distinct health effects. Transfats include:
- "unnatural" cis- and trans monounsaturated fatty acids as they occur in partially hydrogenated fats, but also
- "natural" ones such as vaccenic acid and the conjugated isomers of linoleic acid (CLA) in dairy
about which Mensink et al. write in their 2005 review of the literature, that "it is [still] not clear if effects of ruminant and industrial trans fatty acids on cardiovascular risk are different" from those of the non-ruminant ones (Mensink. 2005).
Before we are taking a closer look at how bad the "bad" unnatural transfats actually are, I would thus like to suggest that we remind ourselves of the benefits of their ruminant cousins.
![]() |
| Contrary to the benefits of supplemental CLA, the beneficial effects of vaccenic acid and other ruminant transfats in dairy are beyond doubt | more |
If you are, as I would hope a
SuppVersity fan and follow all the recent events (which means >9 news items per day) on www.facebook.com/SuppVersity, you will that the evidence to suggest that the effects of hydrogenated vs. ruminated transfats are completely different has been accumulating ever since the publication of Mensink's paper.
Only a couple of days ago, on Friday, to be precise, I posted a blurb about a recent study from the
Konkuk University in Korea, which demonstrated direct anti-cancer effects from the "CLA precursor" vaccenic acid (Lim. 2014). The #1 ruminant transfat in full-fat milk and dairy products (
read more on the
SuppVersity Facebook Page).
![]() |
If you wanted to destroy your body fat, you'd have to consume exclusively the prodiabetic, inflammatory tans-10,
cis-12 isomer | learn more |
Stay away from mixed CLA supplements: Contrary to the health-benefits of their food-borne brethren, the usefulness of the transfats you will find in gel-caps at each and every supplement store are still "controversial" it is clear that "more research is needed before the widely available CLA supplements (racemic mixtures of both isomers with prodiabetic effects; cf. Risérus. 2002) should be advocated as an adjunct to control body weight" (Heer. 2014) - and this is specifically true in view of the opposing effect of cis-9,trans-11 (anti-inflammatory, anti-diabetic | Moloney. 2007) and trans-10,cis-12 (inflammatory | Poirier. 2006) conjugated linoleic acid on blood lipids and glucose metabolism (Halade. 2010)
Now, we've (as so often) been talking about weight loss, and blood lipids. Before we go on, I would thus like to point out that, earlier this year, Nestel et al. have been able to show that lysophosphatidylcholine, lyso-platelet-activating factor, and several phospholipid fatty acids did not only correlate with the number of servings of full-fat dairy foods of 86 overweight and obese subjects with metabolic syndrome, but also with their insulin sensitivity (Nestel. 2014).
Surprise: No evidence to support benefit of reduction of dietary TFA on glucose homeostasisIf we take a look at the corresponding effects of transfats, the picture that emerges is less clear. A recent meta-analysis ofseven randomized, placebo-controlled clinical trials, for example, has shown that an increase in TFA intake from 2.6% to 7.8% of total energy intake did not lead to any significant change in circulating glucose or insulin concentrations (Aronis. 2012). The meta-regression analysis the researchers from the
Harvard Medical School conducted also revealed that there was no dose-response relationship between the amount of transfats their subjects consumed and the corresponding effects on blood glucose and insulin concentrations. In spite of the very real detoriations of the HDL/LDL cholesterol ratio, there is thus, as Aronis et al. rightly point out, "no evidence to support a potential benefit of the reduction of dietary TFA intake on glucose homeostasis." (Aronis. 2012)
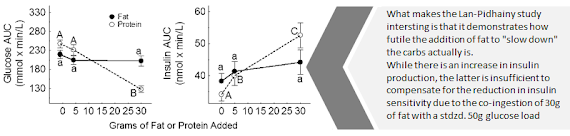
Let's not forget the acute effects!I mentioned them right at the beginning of this article: The acute effects dietary fats can and will have on the blood glucose, insulin and incretin (~satiety hormone) response to a meal.
![]() |
| Figure 2: Blood glucose (mmol/L, left), GIP (pmol/L, top-right), and insulin (mU/L, bottom-right) response to a standardized mashed potato meal 30min after the ingestion of water, olive oil, or both (Gentilcore. 2006) |
As
Figure 2, a compilation of data from a 2006 study by Gentilcore et al. shows, the
pre-ingestion of 30ml olive oil 30 min before a standardized mashed potato meal that was prepared based on 65 g powdered potato and reconstituted with 250 ml water and 20 g glucose (total carbohydrate content of the meal was 61 g) lead to a significant reduction of the postprandial glucose surge (see
Figure 2, left), significant increases in GIP and a prolonged elevation of insulin (
Figure 2, right). As beneficial as the acute reduction in glycemia may seem to a type II diabetic. In the long run it were these prolonged phases of hyperinsulinemia that triggered the development of his diabetes (Marangou. 1996).
The pro-inflammatory effects of high fat meals, of which a recent paper by Mohammed Herieka and Clett Erridge would suggest that they have been underestimated in the common analyses of plasma borne markers of inflammation, such as cytokines and soluble adhesion molecules (Herieka. 2014), on the other hand depend largely on the type of dietary fat that is consumed. While cooking oils and foods that are high in saturated fats appear to have consistent pro-inflammatory effects (Williams. 1999), high MUFA and or omega-3 enriched meals, walnuts, almonds, pistachios and, obviously, fatty fish will ameliorate the postprandial inflammation and exert beneficial effects on the vascular reactivity (West. 2005).
![]() |
| Figure 3: Pro-inflammatory dietary fats are only one of the components that drive the contribution of the postprandial inflammatory response to the self-intensifying circle of metabolic inflammation (Margioris. 2009) |
In conjunction with the caloric value, the glycemic index, and the lipid profile, as well as inter-personal parameters such as obesity, adult onset diabetes and a sedentary life-style, the whole issue of high fat induce post-prandial increases in inflammation and their potential effects on glucose metabolism is yet to complex to be addressed, here. In view of the fact that it is only indirectly related to the topic at hand, you will have to read up on this, yourself. In that, the 2009 paper by Andrew N. Margioris, from which I took
Figure 3, could serve as a starting point (Margioris. 2009).
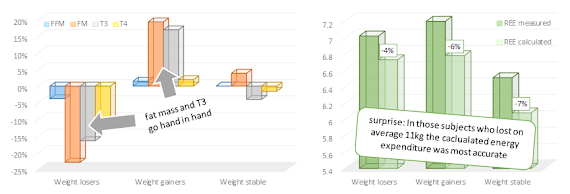
Don't worry if your head feels ready to explode It's about time, we sum things up, anyway. While we certainly have a lot to learn, the contemporary scientific evidence would suggest that...
- the commonly cited negative effects of dietary fat on insulin sensitivity are real - even a high fat, low carb diets will lead to acute reductions in glucose tolerance (Hales. 1963),
- the negative effects on insulin sensitivity are partially mediated by increases in free fatty acids (Roden. 1996),
- the ill health effects of the high fat-induced reduction in glucose tolerance depends on the presence and amount of carbohydrates, as well as the total energy intake and -expenditure and other non-nutrient dependent parameters (Margois. 2009),
- in the postprandial phase, the impaired / slowed influx of glucose and the prolongation of the postprandial hyperinsulinemia may provide an acute relief for people with already elevated blood glucose levels (Gentilcore. 2006), eventually, they will yet promote the development and progression of insulin resistance (Marangou. 1986)
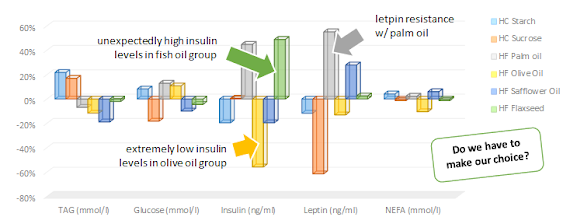
![]() |
| Figure 4: Insulin secretion rates in response to isocaloric meals based water (CONT), palm oil (SFA), olive oil (MUFA) and safflower oil (PUFA) in overweight and obese but otherwise health non-diabetic men (Xiao. 2006) |
the postprandial inflammation that occurs after the ingestion of a high fat meal is problematic for individuals with an already high baseline inflammation (Peairs. 2011),- based on epidemiological evidence it would appear that the replacement of saturated with mono-unsaturated fats will result in long-term improvements in blood glucose management (Gillingham. 2011),
- compared to saturated fat, an increase in polyunsaturated fats improves the acute insulin response to an otherwise isocaloric meal (see Figure 4; safflower vs. olive vs. palm oil in Xiao. 2006),
- the anti-inflammatory effect of omega-3 fatty acids do not produce consistent improvements in blood glucose management (Akinkuolie. 2011),
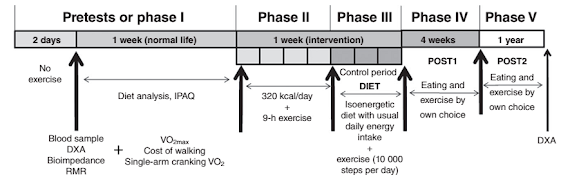
![]() |
| Figure 5: Paleo-lovers listen up! Aside from a higher protein and a sign. lower N6/N3 ratio, the alleged "paleo diet" or rather the diet, Cordain, Eaton & co tell you our ancestors ate had a 50% lower SFA:PUFA ratio (Simopoulos. 2002) |
there are concerns that very high intakes of omega-3 fatty acids (>6g of LCPUFA for months) could lead to reductions in insulin sensitivity similar to those we are seeing with the imbalanced omega-6 intake of the Western diet (Simopoulos. 2002; Mostad. 2006),- the anti-diabetes effects of high(er) PUFA intakes come hand in hand with a pro-obesogenic increase in PPAR-gamma activity similar to, but less pronounced than those of thiazolidinedione-based anti-diabetes drugs like pioglitazone - keyword: "obese, but healthy"
- the existence and even more so the extent of the often-claimed negative effects of transfats on glucose metabolism are dubious (Aronis. 2012); if anything, they occur as long(er) term down-stream effects of more general pro-inflammatory and hyperlipidemic effects of non-ruminate trans fatty acids and the foods that contain them (Remig. 2010), and lastly
- there is accumulating evidence that the natural blend of ruminant transfats in high fat dairy exerts beneficial effects on glucose metabolims (Mensink. 2005; Lim. 2014)
As you will have realized by now, there is no definitive answer to the question, whether fats are good or bad. When it comes to diabetes and insulin resistance, it's not even possible to point with a finger on the bad trans-fats without having to ask yourself, if they aren't yet another scapegoat for a problem that's nor nutrient, but rather food related. A problem for which the overabundance of energy dense nutrient-poor foods is a perfect growth medium.
![]() |
| The superior lean mass and significantly reduced fat gains, Mendes-Netto et al. observed in 2011 with an extreme high carb + low fat diet are a perfect example of the fact you better stay away from fat, when you feel the need to overeat on carbs on a bulk or whenever else | more. |
When it's all said and done, the central message of this extensive analysis is probably that it is simply impossible to look at the effect of dietary fat on glucose homeostasis in man in isolation. In combination with high amounts of 'preferably' fast-digesting carbs dietary fats - specifically saturated ones -
are pro-diabetic villains and their sixfold unsaturated cousins are not a tad better.
In concert with a balanced whole-foods diet, regular physical activity and quality sleep, however, your health and insulin sensitivity are not going to be threatened by the consumption of reasonable amounts of saturated fats and their potentially pro-inflammatory omega-6 cousins whose overabundance and not their inclusion in the modern Western is a highly obesogenic problem (see
Figure 5).
- Akinkuolie, Akintunde O., et al. "Omega-3 polyunsaturated fatty acid and insulin sensitivity: a meta-analysis of randomized controlled trials." Clinical Nutrition 30.6 (2011): 702-707.
- Aranceta, Javier, and Carmen Pérez-Rodrigo. "Recommended dietary reference intakes, nutritional goals and dietary guidelines for fat and fatty acids: a systematic review." British Journal of Nutrition 107.S2 (2012): S8-S22.
- Astrup, Arne, et al. "The role of reducing intakes of saturated fat in the prevention of cardiovascular disease: where does the evidence stand in 2010?." The American journal of clinical nutrition 93.4 (2011): 684-688.
- Benoit, Stephen C., et al. "Palmitic acid mediates hypothalamic insulin resistance by altering PKC-θ subcellular localization in rodents." The Journal of clinical investigation 121.1 (2011): 456.
- Carlson, Susan E., Jane D. Carver, and Stephen G. House. "High fat diets varying in ratios of polyunsaturated to saturated fatty acid and linoleic to linolenic acid: a comparison of rat neural and red cell membrane phospholipids." The Journal of nutrition 116.5 (1986): 718-725.
- den Besten, Gijs, et al. "The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism." Journal of lipid research 54.9 (2013): 2325-2340.
- Flock, Michael R., Jennifer A. Fleming, and Penny M. Kris-Etherton. "Macronutrient replacement options for saturated fat: effects on cardiovascular health." Current opinion in lipidology 25.1 (2014): 67-74.
- Friedberg, Cylla E., et al. "Fish oil and glycemic control in diabetes: a meta-analysis." Diabetes Care 21.4 (1998): 494-500.
- Gadgil, Meghana D., et al. "The Effects of Carbohydrate, Unsaturated Fat, and Protein Intake on Measures of Insulin Sensitivity Results from the OmniHeart Trial." Diabetes care 36.5 (2013): 1132-1137.
- Gentilcore, Diana, et al. "Effects of fat on gastric emptying of and the glycemic, insulin, and incretin responses to a carbohydrate meal in type 2 diabetes." Journal of Clinical Endocrinology & Metabolism 91.6 (2006): 2062-2067.
- Gillingham, Leah G., Sydney Harris-Janz, and Peter JH Jones. "Dietary monounsaturated fatty acids are protective against metabolic syndrome and cardiovascular disease risk factors." Lipids 46.3 (2011): 209-228.
- Grygiel-Górniak, Bogna. "Peroxisome proliferator-activated receptors and their ligands: nutritional and clinical implications-a review." Nutrition journal 13.1 (2014): 17.
- Halade, Ganesh V., Md M. Rahman, and Gabriel Fernandes. "Differential effects of conjugated linoleic acid isomers in insulin-resistant female C57Bl/6J mice." The Journal of nutritional biochemistry 21.4 (2010): 332-337.
- Hales, C. N., and P. J. Randle. "Effects of low-carbohydrate diet and diabetes mellitus on plasma concentrations of glucose, non-esterified fatty acid, and insulin during oral glucose-tolerance tests." The Lancet 281.7285 (1963): 790-794.
- Harvey, Kevin A., et al. "Long-chain saturated fatty acids induce pro-inflammatory responses and impact endothelial cell growth." Clinical Nutrition 29.4 (2010): 492-500.
- Herieka, Mohammed, and Clett Erridge. "High‐fat meal induced postprandial inflammation." Molecular nutrition & food research 58.1 (2014): 136-146.
- Kennedy, Arion, et al. "Saturated fatty acid-mediated inflammation and insulin resistance in adipose tissue: mechanisms of action and implications." The Journal of nutrition 139.1 (2009): 1-4.
- Khan, Mehmood A., John V. St Peter, and Jay L. Xue. "A prospective, randomized comparison of the metabolic effects of pioglitazone or rosiglitazone in patients with type 2 diabetes who were previously treated with troglitazone." Diabetes Care 25.4 (2002): 708-711.
- Kien, C. Lawrence, et al. "Substituting dietary monounsaturated fat for saturated fat is associated with increased daily physical activity and resting energy expenditure and with changes in mood." The American journal of clinical nutrition 97.4 (2013): 689-697.
- Kimura, Ikuo, et al. "The gut microbiota suppresses insulin-mediated fat accumulation via the short-chain fatty acid receptor GPR43." Nature communications 4 (2013): 1829.
- Kota, Bhavani Prasad, Tom Hsun-Wei Huang, and Basil D. Roufogalis. "An overview on biological mechanisms of PPARs." Pharmacological Research 51.2 (2005): 85-94.
- Lombardo, Yolanda B., and Adriana G. Chicco. "Effects of dietary polyunsaturated n-3 fatty acids on dyslipidemia and insulin resistance in rodents and humans. A review." The Journal of nutritional biochemistry 17.1 (2006): 1-13.
- Lemaitre, Rozenn N., et al. "Cell membrane trans-fatty acids and the risk of primary cardiac arrest." Circulation 105.6 (2002): 697-701.
- Lovejoy, Jennifer C., et al. "Effects of diets enriched in saturated (palmitic), monounsaturated (oleic), or trans (elaidic) fatty acids on insulin sensitivity and substrate oxidation in healthy adults." Diabetes care 25.8 (2002): 1283-1288.
- Marangou, A. G., et al. "Metabolic consequences of prolonged hyperinsulinemia in humans: evidence for induction of insulin insensitivity." Diabetes 35.12 (1986): 1383-1389.
- Margioris, Andrew N. "Fatty acids and postprandial inflammation." Current Opinion in Clinical Nutrition & Metabolic Care 12.2 (2009): 129-137.
- McManus, Ruth M., et al. "A comparison of the effects of n-3 fatty acids from linseed oil and fish oil in well-controlled type II diabetes." Diabetes Care 19.5 (1996): 463-467.
- Mendes-Netto, R. S., et al. "Effect of the dietary glycid/lipid calorie ratio on the nitrogen balance and body composition of bodybuilders." Nutrire-Revista da Sociedade Brasileira de Alimentação e Nutrição 36.1 (2011): 137-150.
- Mensink, Ronald P. "Metabolic and health effects of isomeric fatty acids." Current opinion in lipidology 16.1 (2005): 27-30.
- Kabir, Morvarid, et al. "Treatment for 2 mo with n− 3 polyunsaturated fatty acids reduces adiposity and some atherogenic factors but does not improve insulin sensitivity in women with type 2 diabetes: a randomized controlled study." The American journal of clinical nutrition 86.6 (2007): 1670-1679.
- Lee, C., et al. "Fish consumption, insulin sensitivity and beta-cell function in the Insulin Resistance Atherosclerosis Study (IRAS)." Nutrition, Metabolism and Cardiovascular Diseases 23.9 (2013): 829-835.
- Lim, Ji-Na, et al. "trans-11 18: 1 Vaccenic Acid (TVA) Has a Direct Anti-Carcinogenic Effect on MCF-7 Human Mammary Adenocarcinoma Cells." Nutrients 6.2 (2014): 627-636.
- Mahendran, Yuvaraj, et al. "Association of erythrocyte membrane fatty acids with changes in glycemia and risk of type 2 diabetes." The American journal of clinical nutrition 99.1 (2014): 79-85.
- Montori, Victor M., et al. "Fish oil supplementation in type 2 diabetes: a quantitative systematic review." Diabetes Care 23.9 (2000): 1407-1415.
- Mostad, Ingrid L., et al. "Effects of n− 3 fatty acids in subjects with type 2 diabetes: reduction of insulin sensitivity and time-dependent alteration from carbohydrate to fat oxidation." The American journal of clinical nutrition 84.3 (2006): 540-550.
- Peairs, Abigail D., Janet W. Rankin, and Yong Woo Lee. "Effects of acute ingestion of different fats on oxidative stress and inflammation in overweight and obese adults." Nutr J 10.1 (2011): 122.
- Poirier, Hélène, et al. "Nutritional supplementation with trans-10, cis-12–conjugated linoleic acid induces inflammation of white adipose tissue." Diabetes 55.6 (2006): 1634-1641.
- Popp-Snijders, C., et al. "Dietary supplementation of omega-3 polyunsaturated fatty acids improves insulin sensitivity in non-insulin-dependent diabetes." Diabetes Research (Edinburgh, Scotland) 4.3 (1987): 141-147.
- Remig, Valentina, et al. "Trans Fats in America: A Review of Their Use, Consumption, Health Implications, and Regulation." Journal of the American Dietetic Association 110.4 (2010): 585-592.
- Risérus, Ulf, et al. "Treatment with dietary trans10cis12 conjugated linoleic acid causes isomer-specific insulin resistance in obese men with the metabolic syndrome." Diabetes care 25.9 (2002): 1516-1521.
- Risérus, Ulf. "Fatty acids and insulin sensitivity." Current Opinion in Clinical Nutrition & Metabolic Care 11.2 (2008): 100-105.
- Roden, Michael, et al. "Mechanism of free fatty acid-induced insulin resistance in humans." Journal of Clinical Investigation 97.12 (1996): 2859.
- Sawada, Keisuke, et al. "Ameliorative effects of polyunsaturated fatty acids against palmitic acid-induced insulin resistance in L6 skeletal muscle cells." Lipids Health Dis 11.1 (2012): 36-44.
- Simopoulos, Artemis P. "The importance of the ratio of omega-6/omega-3 essential fatty acids." Biomedicine & pharmacotherapy 56.8 (2002): 365-379.
- Schwingshackl, L., B. Strasser, and G. Hoffmann. "Effects of monounsaturated fatty acids on glycaemic control in patients with abnormal glucose metabolism: a systematic review and meta-analysis." Annals of Nutrition and Metabolism 58.4 (2011): 290-296.
- Vessby, Bengt, et al. "Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: The KANWU Study." Diabetologia 44.3 (2001): 312-319.
- Williams, Michael JA, et al. "Impaired endothelial function following a meal rich in used cooking fat." Journal of the American College of Cardiology 33.4 (1999): 1050-1055.
- Xiao, C., et al. "Differential effects of monounsaturated, polyunsaturated and saturated fat ingestion on glucose-stimulated insulin secretion, sensitivity and clearance in overweight and obese, non-diabetic humans." Diabetologia 49.6 (2006): 1371-1379.

![]()