|
| The press release that accompanied the publication of a study from the Augusta University seems to promote baking soda as a panacea for every (auto-) immune/inflammation-related disease. |
Well, the mechanism that is introduced in the press release does not seem to be totally absurd. The fact that a temporary alkalization of the otherwise acidic chyme in the stomach will trigger for the production of an increased amount of stomach acid has been known for decades (it is also why classic antacids usually make heartburn worse when used more than occasionally | Maton 1999).
You can learn more about bicarbonate and pH-buffers at the SuppVersity
Wait!? Polarization? That's a property of waves, not of cells, isn't it?
If we go by the physics definition, polarization is "the action of restricting the vibrations of a transverse wave, especially light, wholly or partially to one direction". For us, however, it's the more general term that's relevant, here: "division into two sharply contrasting groups or sets of opinions or beliefs." When it comes to Donald Trump, for example, you can clearly observe a polarization of the US society - with supporters and opponents being "two sharply contrasting groups".
 |
| Figure 1: Overview of how different stimuli, e.g. TNF-alpha will trigger the commitment of Th0 (=naive T-helper cells/lymphocytes) to Th1, Th2, Th17 and Treg cells (as published on selfHacked.com; original source unknown). These T-cells, are the first responders, they attack and kill intruders that will then be 'eaten' by macrophages. |
I don't intend to go into more detail here because, for our purposes, it shall suffice to know that the same mechanisms that govern the polarization of T-cells will also determine the fate of the macrophages that will appear on the scene, whence the T-cells did their job (on nobelprize.org you can find a relatively simple explanation of the inner workings of the immune system) and promote the progression of pro- or anti-inflammatory immune responses via TNF-alpha and IL-10 release, respectively. In an (over-)simplified model, the Th1/Th2 and the M1/M2 (M=macrophages) ratios can thus both be used as proxies of whether the immune system is in an M1/inhibit-type mode,primed to defend the host, or in an M2/heal-type mode, focussing on the repair and replacement of lost or defected tissue to maintain host homeostasis (Mills 2015a).
The vagal nerve, again and a new role for our mesothelial cells in the gut
As previously hinted at, it depends on the presence of certain signaling molecules like TNF-alpha or IL-6 (to name just the two best-known factors) whether naive T-cells and macrophages will be configured to become Th1/M1 or Th2/M2 cells.... and that's where the press release starts to fail us and we have to go to the actual study by Sarah C. Ray and colleagues from the Augusta University (Ray 2018) to understand or rather rationalize how the sudden in- and slow decrease of gastric pH will do what the author of the press release calls "tell the fist-sized organ [thymus] that there's no need to mount a protective immune response" (press release).
 |
| Figure 2: The cholinergic tone determines immune homeostasis, either shifting the balance toward tolerance (normal to enhanced tone) or inflammation (decreased tone | Browning 2017). |
This involvement of the vagal nerve is not new as it has been observed and described as a main regulator of the cholinergic anti-inflammatory pathway and thus mediator of immune homeostasis before (the vagus nerve has, in fact, been implicated as key-player in the interaction between the gut microbiome and the immune system and even appetite and mood, too | cf. Browning 2017).
Why did the scientists do their study and what exactly were they studying? Ray et al. drew on evidence fro a number of small clinical trials as well as experimental models which indicate that supplementation with oral sodium bicarbonate (NaHCO3) may slow the decline in kidney function in chronic kidney disease (CKD) patients. That is relevant to the topic of auto-immune diseases because the #1 hypothesis to explain the beneficial effects scientists have observed in this patient group is... you guessed it: inflammation. Accordingly, the scientists from the Augusta University set up a series of experiments to investigate if and to which extent baking soda, sodium bicarbonate, or NaHCO3, which all refer to the same white powder (not to be confused with other white powders ;-) may have previously overlooked fundamental anti-inflammatory effects that could be mediated via a similar or different pathways within the gastric <> spleen axis that has recently received a lot of attention for its role in the interaction between the microbiome and our immune system.
In their study, Ray et al. started with a rodent model - more specifically, the researchers chose Dahl salt-sensitive (SS) rats, in which significant inflammation is known to develop very early in life and keeps increasing from 'low' to 'extreme' as they age. |
| Figure 3: The ratio of pro-inflammatory M1 to anti-inflammatory M2 monocytes (this is a simplification) was almost reversed by 14 days w/ 0.1 mol of NaHCO3 in their drinking water compared to vehicle control in both the kidney's and spleen - with a clear trend to a less inflammatory M1/M2 ratio that was below 1 (Ray 2018). |
- a significant (p < 0.01) decrease in TNFa–expressing macrophages (M1-polarized macrophages) and...
- a significant increase in the anti-inflammatory IL-10–expressing macrophages (M2-polarized macrophages) ...
Sorry, off topic: If the quotes I used in the last paragraph remind you of the bearded guy in "Il était une fois... la vie", also known as "Micro Patrol", "Es war einmal das Leben" or "Seimei no Kagaku: Mikuropatorōru", your early childhood memories may actually help you understand what macrophages are - there's a screengrab of the way they looked in this excellent educative TV show on the left... it's funny that this image pops up in my head even 25 years after I used to watch this show (let me know if you loved it, too)... but now back to the topic at hand ;-)
For those who cannot wait: In humans, 2g/250ml of NaHCO3 worked wonders
If we do the math, those 0.01 M of bicarbonate translate to 610mg of HCO3. Given the fact that NaHCO3 has a ~1:3 ratio of Na to HCO3, this should be ~840mg of baking soda. Translation to humans is difficult because we'd have to take into account the rodent weight and their intake patterns. For those who cannot wait for dosage suggestions, I can yet already spoiler that Ray et al. used 2g of bicarbonate per 250ml in their follow-up human experiment (see below).
How the signals get from the gut to the spleen and why you should abstain from PPIs if you want to benefit: At least the hitherto available evidence suggests that the effect could be mediated by the activation of the cholinergic anti-inflammatory pathway, the spleen will then react to by switching the immune cells from "fight"- to "guard"-mode come directly from the mesothelial cells in the abdominal cavity and are triggered by the sudden increase in pH. The cells line many body cavities in our body, including the digestive tract, where they cover the exterior of the organs and have previously been thought to primarily keep the organs from rubbing together. With their little fingers (=microvilli) that reach into the organs, though, they can also be seen as biosensors that warn the organs they cover that there is an invader and an immune response is needed.
What exactly it is that these cells respond to is not 100% clear, but the inhibitory effect of the administration of pretreatment with the proton-pump inhibitor (PPI) Esomeprazole suggests that a drop in pH alone is not sufficient, only if it's followed by a gradual increase in stomach acid effects can be observed... theoretically, however, there could be completely different mechanism and/or feedback loop may be at play when it comes to PPIs.
With the effects on the M1/M2 ratio occurring both, locally (kidney, spleen) and systemically (in the blood, not shown in Figure 1), the rodent experiment provided exactly the sought after initial evidence that the researchers were onto something that could be relevant way beyond chronic kidney disease. In fact, the repolarization of an out-of-control immune defense is often thought of as the golden grail of treating all sorts of auto-immune diseases. |
| Both, the inhibition of cholinergic transmission with MLA and the inhibition of the stomach acid rebound with PPIs weakens the effect on NaHCO3 in the rodent model. |
 |
| Figure 5: M1- or M2-dominant immune responses are associated with specific diseases (Mills 2012). |
Can bicarbonate treat auto-immune diseases from arthritis to multiple-sclerosis by setting the 'M1/M2 seesaw' back in motion and thus restoring immune balance?
It would be downright dishonest to make such a claim based on the study at hand - and yet, that's pretty much what the press release seems to do. From my good friend, Carl Lanore, the host of Super Human Radio (superhumanradio.net), I know that he's going to have one of the authors on the show on Monday; and, according to Carl, the authors are really unhappy with the way the study was depicted in the press release, too.
 |
| In an interview with my friend Carl Lanore for Super Human Radio Dr. O'Connor explains why he wasn't happy with the press release that caused all the turmoil, either - listen! |
So what does the study tell us, then?
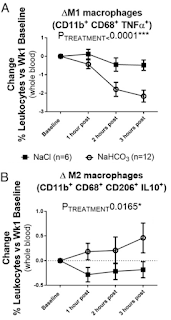
The one thing the experiment in humans tells us is that the ingestion of 2g of bicarbonate dissolved in 250ml of water can have acute, systemic and, in view of the fact that the inflammatory effects accumulated over hours after the subjects consumed the drink, long-lasting anti-inflammatory effects on the immune system.
This effect is, as the scientists explain in the discussion of the results due to a (re-)polarization from M1 to M2 macrophages and increased FOXP3+ CD4+ T regulatory cells (Tregs) of which you may remember from Figure 1 that they regulate (hence T regulatory cells) the immune response and (not shown in Figure 1) have been implicated as potential targets for the treatment of auto-immune diseases, in which they fail to do their job of telling the autoimmune T-cells to behave (see Figure 6 | Grant 2015).
 |
| Figure 6: Regulatory T cell defects in autoimmunity. In health, Tregs maintain tolerance by exerting suppression of effector T cells. In organ-specific autoimmune disease, Tregs fail to suppress autoreactive effector T cells, therefore leading to target cell death. Reported reasons for this include inadequate numbers of Tregs, impaired suppressive ability, Treg conversion into effector cells and resistance of effector T cells to Treg-mediated suppression (Grant 2015). |
- be able to protect you from developing a Treg-malfunction, which appears to be closely related to the chronic inflammatory state, the scientists found to be ameliorated in response to the bicarbonate ingestion, and
- maybe even restore normal Treg function so that they could do their job(s) and shut the autoreactive T-cells that are attacking one's own organs in autoimmune diseases down.
"[...] may be beneficial in a wide variety of disease states that involve pathological activation of the immune system, including allergy, asthma, multiple sclerosis, graft versus host disease, diabetes, and hypertension as well as many others" (Ray 2018).could be confounded by the profound decrease of TNA-alpha - the #1 among cytokines scientists have linked to the development/progression of a "broad range of disease states, including rheumatoid arthritis, cardiovascular disease, atherosclerosis, irritable bowel disease, type 2 diabetes, and neurodegenerative diseases" (Ray 2018).
If and to which extent and in which conditions bicarbonates anti-inflammatory effects will become physiologically relevant is, however, as of now absolutely unknown (don't forget that).
Ok, that's not 100% true. For chronic kidney disease, which is likewise characterized by high TNF-alpha levels and chronic inflammation, there's plenty of evidence from both animal and human studies that the provision of sodium bicarbonate, administered in similarly small dosages as in the study at hand (just a reminder: 1x2g/250ml water) can at least slow down the progression of the disease (Susantitaphong 2012).
It's yet not just the fact that most scientists point towards the anti-acidogenic effects of bicarbonate as the underlying mechanism for the indisputable benefits of NaHCO3 supplements in CKD patients that raises the question whether we'd see similar benefits in autoimmune diseases - let alone (and again that's only what the press release, not the study implies) the immune response to certain foods you eat.
 |
| Figure 7: M1/inhibit or M2/heal-dominant macrophage responses (or mixtures) can each be beneficial or detrimental depending on the disease circumstance. For example, M1/Th1-dominant responses are required to fight many infections (left). But, M1/Th1 responses are also causative of destructive inflammatory conditions in the brain and in atherosclerosis (right | Mills 2015b) - as previously highlighted, it's a working seesaw (=balance) you should aim for. |
"[...] provide a cheap, relatively safe, effective, and easily accessible and/or noninvasive method to activate cholinergic anti-inflammatory pathways in humans [which could] be of benefit to patients suffering from a multitude of inflammatory disease states [which] could potentially have significant clinical application to the treatment of human disease" (my emphasis in Ray 2018).Unlike the press release, though, the scientists are also prudent enough to highlight that: "Future studies testing the efficacy of oral NaHCO3 to limit injury in models of inflammatory disease will be required to determine the therapeutic potential of this stimuli" (Ray 2018) - and if we're honest this is, if anything, the only 100% reliable take-home message of the study at hand.
There's the practical reason, which holds true even if we assumed that the, as of yet not even investigated interaction with food, everyone seems to focus on in the discussion on the SuppVersity News and elsewhere, actually exists:
- There's no way to guess the optimal timespan between the ingestion of NaHCO3 and the subsequent meal. So, there may be the interaction between foods, bicarbonate, and inflammation the press release seems to hint at, but (a) the study at hand did not even test for such an interaction and (b) we only know that the anti-inflammatory effect kept improving for the complete 3h measuring period in the subjects... if you'd best ingest the food at the peak level of M2 macrophages, of which the graphs in Figure 8 suggest that it may be 4-5h after the ingestion of the bicarbonate solution, or right before a meal is thus at best an (almost un-)educated guess.
- It is thus not just unclear if NaHCO3 would indeed help with autoimmune disease. In view of the fact that we don't know for sure how NaHCO3 exerts its anti-inflammatory effects on the immune system, how profound they are and how long they will last, it is, moreover, even possible that anything that that would go beyond what the authors in another quote from the infamous press release call "pushing [the immune response] toward one side by giving an anti-inflammatory stimulus" (I previously called that fixing the seesaw) could have serious unwanted side effects.
Note: I don't say it's likely that you would encounter side effects, but even O'Connors (alleged) statement that "[bicarbonate] is potentially a really safe way to treat inflammatory disease" (press release) still has the status of a hypothesis and requires testing in all sorts of different scenarios. I mean, you know that I am a huge fan of bicarbonate and have been using more than 2g regularly over the past years without any side effects, but that's an N=1 scenario that won't tell you anything about people with pre-existing health conditions that make them susceptible to infection, allergies, or even cancer... Why would I mention the three of them? Well, in the unfortunate case that there are problems due a chronic elevation of M2 (vs. M1) those would be related to the impairment of the early phase response to infections (like in the throat or intestine) to an exacerbation of food or contact allergies (Suzuki 2017), or - even worse - the promotion of proliferation not just of healthy cells, but also of cancer cells (Mills 2012 | all are also visualized in Figure 7 from Mills 2015b).
- Browning, Kirsteen N., Simon Verheijden, and Guy E. Boeckxstaens. "The vagus nerve in appetite regulation, mood, and intestinal inflammation." Gastroenterology 152.4 (2017): 730-744.
- Grant, Charlotte R., et al. "Regulatory T-cells in autoimmune diseases: challenges, controversies and—yet—unanswered questions." Autoimmunity reviews 14.2 (2015): 105-116.
- Maton, Paul N., and Michael E. Burton. "Antacids revisited." Drugs 57.6 (1999): 855-870.
- Mills, Charles. "M1 and M2 macrophages: oracles of health and disease." Critical Reviews™ in Immunology 32.6 (2012).
- Mills, Charles D., Laurel L. Lenz, and Klaus Ley. "Macrophages at the fork in the road to health or disease." Frontiers in immunology 6 (2015a): 59.
- Mills, Charles Dudley. "Anatomy of a discovery: m1 and m2 macrophages." Frontiers in immunology 6 (2015b): 212.
- Ray, Sarah C., et al. "Oral NaHCO3 Activates a Splenic Anti-Inflammatory Pathway: Evidence That Cholinergic Signals Are Transmitted via Mesothelial Cells." The Journal of Immunology (2018): ji1701605.
- Susantitaphong, Paweena, et al. "Short-and long-term effects of alkali therapy in chronic kidney disease: a systematic review." American journal of nephrology 35.6 (2012): 540-547.
- Suzuki, Kotaro, et al. "Roles of alternatively activated M2 macrophages in allergic contact dermatitis." Allergology International 66.3 (2017): 392-397.