|
| Vitamin A is not exactly known for being an anti-diabetes vitamin. If anything people will associate it with skin health... and SuppVersity Readers probably with anti-cellulite treatments | learn more |
In view of the misleading news about the "involvement" of retinol binding proteins in the etiology of the diabesity epidemic and the bullocks about the negative effects of vitamin A on vitamin D, the vast majority of health junkies all over the web will probably associate high vitamin A intakes with insulin resistance, not -sensitivity.
You can learn more about this topic at the SuppVersity
As the scientists from the University of Alberta point out, the increased hepatic and the decreased plasma and retina vitamin A levels clearly "suggest a defect in the transport of the vitamin from the liver" - a defect of which it's not unlikely that it is the cause of the previously mentioned increases in retinol binding protein 4 (RBP4) that are so characteristic of the average overweight type II diabetic (Cho. 2006). Whether this problem can be resolved by the provision of supplemental vitamin A is albeit highly controversial.
 |
| Vitamin A is involved in body fat control (Bonet. 2003) |
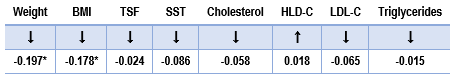
There are other things vitamin A can day for the diabetic patient -- It can promote wound healing, for example (Seifter. 1981). It can (at least in rodent trials) reduce the expression of resistin (Felipe. 2004), which is associated with increased levels of "bad" oxidized LDL cholesterol and is in itself a biomarker for the risk of heart failure (Salam. 2013; Takeishi. 2013). When it's administered with zinc at a daily dose of 25,000IU retinol can the improve serum apoprotein A-I, apoprotein B and the apoprotein B/apoprotein A-I ratio in patients with type I diabetes (Shidfar. 2013) and may thus directly reduce their heart disease risk.
Whether the potential side effects will yet occur in subjects, in whom the elevated glucose levels are adequately controlled is yet questionable. The results a group of researchers from the Ankara University presented in 2002 article in the peer-reviewed scientific journal Cell Biochemistry and Function, for example, would suggest that the addition of supplemental vitamin A to the standard insulin therapy in type II diabetes will not just help to keep the exuberant glucose levels in check, it may also blunt the oxidative reactions in diabetic heart and may thus "provide more benefits than use of either agent alone in the treatment of the "general characteristics of diabetes and the maintenance of antioxidant defense of diabetic heart and thus in the reduction of peroxidative stress-induced cardiac injury" (Zobalı. 2002).  |
| Figure 1: Vitamin A affects several key steps in glucose metabolism (highlighted by dark arrows Berdainer. 2001) |
As Berdainer et al. point out, "glucose-stimulated insulin secretion is a complex process that requires the metabolism of glucose and the mitochondrial production of ATP" (Berdanier. 2001) - a process, in which the rate limiting enzymes that are regulated by retinoic acid (see Figure 1).
 |
| The vitamin A metabolite all-trans-retinoic acid is a real "anti-metabolic syndrome"-agent (Bonet. 2012) |
In conjunction with its ability to "brown" white fat cells and thus turn fat stores into fat furnaces (Mercader. 2006), the increases in skeletal muscle fatty oxidation will obviously also have secondary anti-diabetic effects (warning: ATRA is significantly more toxic than vitamin A and liposomal delivery reduces, but does not abolish these effects; cf. Ozpolat. 2003).
In that, the negative association between vitamin A and non-alcoholic fatty liver disease José Botella-Carretero et al. observed in morbidly obese subjects just another component of the under-appreciated involvement of vitamin A in the etiology of diabetes (Botella-Carretero. 2010) - an involvement of which we yet don't know whether it's causally, corellative or both.
Just as an aside: Vitamin A will also increase the expression of the master anti-oxidant glutathione in muscle tissue and promote the survival skeletal muscle precursor cells (El Haddad. 2012). It is necessary to preserve protein (Esteban-Pretel. 2010). And protects the muscle from the catabolic effects of corticosteroid overload (Aubry. 2009). Not glucose related, but not bad either, right?
Bottom line: There is little doubt that low vitamin A levels will contribute to the development of insulin resistance - both directly, by its negative effect on the pancreatic insulin production, and its insulin-induced glucose uptake in skeletal muscle tissues, as well as indirectly by its pro-obesogenic effects, and reductions in fatty acid oxidation and brown adipose tissue activity.
What is questionable, though, is whether the provision of supplemental vitamin A will have any direct or indirect beneficial effects on glucose metabolism in the average lean vitamin A sufficient individual and/or vitamin A deficient (pre-)diabetics. Against that background I would recommend to keep an eye on an adequate dietary vitamin A intake from eggs, dairy, butter, meat, fish and the occasional serving of liver and / or supplemental retinyl palmitate (e.g. 10,000 IU; 2-3x per week).
What is questionable, though, is whether the provision of supplemental vitamin A will have any direct or indirect beneficial effects on glucose metabolism in the average lean vitamin A sufficient individual and/or vitamin A deficient (pre-)diabetics. Against that background I would recommend to keep an eye on an adequate dietary vitamin A intake from eggs, dairy, butter, meat, fish and the occasional serving of liver and / or supplemental retinyl palmitate (e.g. 10,000 IU; 2-3x per week).
- Amengual, Jaume, et al. "Retinoic acid treatment enhances lipid oxidation and inhibits lipid biosynthesis capacities in the liver of mice." Cellular Physiology and Biochemistry 25.6 (2010): 657-666.
- Aubry, Evelyne M., and Alex Odermatt. "Retinoic acid reduces glucocorticoid sensitivity in C2C12 myotubes by decreasing 11β-hydroxysteroid dehydrogenase type 1 and glucocorticoid receptor activities." Endocrinology 150.6 (2009): 2700-2708.
- Basu, T. K., W. J. Tze, and J. Leichter. "Serum vitamin A and retinol-binding protein in patients with insulin-dependent diabetes mellitus." The American journal of clinical nutrition 50.2 (1989): 329-331.
- Basu, Tapan K., and Carlotta Basualdo. "Vitamin A homeostasis and diabetes mellitus." Nutrition 13.9 (1997): 804-806.
- Berdanier, Carolyn D., et al. "Role of vitamin A in mitochondrial gene expression." Diabetes research and clinical practice 54 (2001): S11-S27.
- Bonet, M. L., et al. "Vitamin A and the regulation of fat reserves." Cellular and Molecular Life Sciences CMLS 60.7 (2003): 1311-1321.
- Bonet, M. Luisa, Joan Ribot, and Andreu Palou. "Lipid metabolism in mammalian tissues and its control by retinoic acid." Biochimica et Biophysica Acta (BBA)-Molecular and Cell Biology of Lipids 1821.1 (2012): 177-189.
- Botella-Carretero, José I., et al. "Retinol and α-tocopherol in morbid obesity and nonalcoholic fatty liver disease." Obesity surgery 20.1 (2010): 69-76.
- Chertow, B. S., et al. "Effects of vitamin A deficiency and repletion on rat insulin secretion in vivo and in vitro from isolated islets." Journal of clinical Investigation 79.1 (1987): 163.
- Chertow, B. S., et al. "Effects of vitamin A deficiency and repletion on rat glucagon secretion." Pancreas 9.4 (1994): 475-484.
- Cho, Young Min, et al. "Plasma retinol-binding protein-4 concentrations are elevated in human subjects with impaired glucose tolerance and type 2 diabetes." Diabetes care 29.11 (2006): 2457-2461.
- El Haddad, Marina, et al. "Glutathione peroxidase 3, a new retinoid target gene, is crucial for human skeletal muscle precursor cell survival." Journal of cell science 125.24 (2012): 6147-6156.
- Esteban-Pretel, Guillermo, et al. "Vitamin A deficiency increases protein catabolism and induces urea cycle enzymes in rats." The Journal of nutrition 140.4 (2010): 792-798.
- Farhangi, Mahdieh Abbasalizad, et al. "Vitamin A supplementation, serum lipids, liver enzymes and C-reactive protein concentrations in obese women of reproductive age." Annals of clinical biochemistry 50.1 (2013): 25-30.
- Felipe, Francisco, et al. "Modulation of resistin expression by retinoic acid and vitamin A status." Diabetes 53.4 (2004): 882-889.
- Lu, Jing, et al. "The metabolic availability of vitamin A is decreased at the onset of diabetes in BB rats." The Journal of nutrition 130.8 (2000): 1958-1962.
- Mercader, Josep, et al. "Remodeling of white adipose tissue after retinoic acid administration in mice." Endocrinology 147.11 (2006): 5325-5332.
- Ozpolat, Bulent, et al. "Pharmacokinetics of intravenously administered liposomal all-trans-retinoic acid (ATRA) and orally administered ATRA in healthy volunteers." J Pharm Pharm Sci 6.2 (2003): 292-301.
- Salam, Gazbar, et al. "Relationship between Oxidized-LDL and Resistin Levels in Obese Diabetic Subjects." (2013).
- Seifter, E., et al. "Impaired wound healing in streptozotocin diabetes. Prevention by supplemental vitamin A." Annals of surgery 194.1 (1981): 42.
- Shidfar, Farzad, et al. "Effects of combination of zinc and vitamin A supplementation on serum fasting blood sugar, insulin, apoprotein B and apoprotein AI in patients with type I diabetes." International journal of food sciences and nutrition 61.2 (2010): 182-191.
- Sleeman, Mark W., et al. "Retinoic acid stimulates glucose transporter expression in L6 muscle cells." Molecular and cellular endocrinology 108.1 (1995): 161-167.
- Takeishi, Y. "Resistin Is a Novel Biomarker for a Risk of Heart Failure." J Cardiovasc Dis Diagn 1.122 (2013): 2.
- Tuitoek, P. J., et al. "Streptozotocin-induced diabetes in rats is associated with impaired metabolic availability of vitamin A (retinol)." British Journal of Nutrition 75.04 (1996): 615-622.
- Tungtrongchitr, Rungsunn, et al. "The relationships between anthropometric measurements, serum vitamin A and E concentrations and lipid profiles in overweight and obese subjects." Asia Pacific J Clin Nutr 12.1 (2003): 73-79.
- Zobalı, Fulya, et al. "Effects of vitamin A and insulin on the antioxidative state of diabetic rat heart: a comparison study with combination treatment." Cell biochemistry and function 20.2 (2002): 75-80.