Can this be? Can your "gluten intolerance" really be in your head? Certainly it can, it's what scientists call a nocebo effect: A situation, where a harmless substance taken by a patient is associated with harmful effects due to negative expectations or the psychological condition of the patient.
But wheat is no harmless substance, right?
Certainly not. At least not for those people who suffer from celiac disease. As far as the ever-spreading gluten-intolerance is concerned, though, more and more scientists voice concerns over the ever-increasing number of self-diagnosed gluten-intolerant individuals strike one food item after the other from their already short list of "gluten kosher" foods.
 |
| Social influences on Australian "wheat avoiders" (Golley. 2014) |
"[T]his research suggests that self-ascriptive looping results in a greatly expanded illness prototype, and that gluten-free individuals promote a broadened illness prototype and self-diagnosis to their friends and families. Some work to promote the diet further. As a result, self-ascriptive looping can function as one vector in the diet's growing popularity." (Moore. 2014).The so-called looping effect describes how categories are continually redefined as the people within them change. The group of "gluten intolerant" individuals, once only celiacs, has thus over time transformed into an amalgam with celiac patients on the one end and real hypochondriacs on the other end of the extreme. And they all have one thing in common. For each of them, his or hear gluten intolerance is absolutely real.
In view of the way this illness prototype or rather its contemporary realization is constantly changing it's no wonder that it has lost all resemblance to what doctors call "gluten intolerance". The logical consequence: Patients feel misunderstood and blame their "doctors for their failure to correctly diagnose the problem." (Moore. 2014)
The illness is real, and so are the risks
In the end, it's thus not a question of who's wrong and who's right. For the "patients" who have now become their own doctors their illness is absolutely real. The previously asked question, whether wheat is a harmless substance or not is thus no longer practically relevant for them and they are willing to pay the price - literally that is by paying significantly more money for (oftentimes) nutritiously inferior foods from the "gluten-free" industry (Hallert. 1998; Long. 2010).
What about the physiological side?
As the previous remarks have shown, there is little doubt that the contemporary trend towards "gluten-free" diets is a socio-psychological phenomonen that's not (yet?) rooted in conclusive scientific evidence that would point towards general detrimental effects of wheat consumption on non-celiac human beings (Brouns. 2013).
- Wheat amylase trypsin inhibitors may drive intestinal inflammation via activation of toll-like receptor 4 -- Yvonne Junker et al. report in a 2012 paper that the natural α-amylase/trypsin inhibitors in wheat "may fuel inflammation and immune reactions in other intestinal and non-intestinal immune disorders." (Junker. 2012).
- Auto-immune reactions could be triggered without the expression of T-cell specific antigens -- Using recent evidence from celiac patients as an example, Ludvig M. Sollid & Bana Jabri argue that the constant exposure to certain immuno-modulating substances such as gluten, could be exogenous factors which "might be identified as drivers of autoimmune processes, in particular when evidence for T cells with specificity for self antigens driving the disease is lacking." (Sollid. 2013)
- Low-fermentable, poorly-absorbed, short-chain carbohydrates could contribute to symptoms (at least those related to IBS) experienced by non-celiac-gluten-sensitivity patients -- With the low-fermentable, poorly-absorbed, short-chain carbohydrates, i.e. fermentable oligo-, di-, and mono-saccharides and polyols, aka FODMAPs an international group of scientists suspects another of the blogosphere's usual suspects may be to blame.
The data from a 7-day low FODMAP study does actually appear to support a relevant interaction of FODMAPs and gluten sensitivity (Biesiekierski. 2013).![]()
Figure 2: A low FODMAP diet will progressively reduce the symptoms of NCGS (Biesiekierski. 2013)
The results do yet require experimental verification and further research should try to reveal the underlying mechanism which could explain the reduction in gluten sensitivity in response to the low FODMAP diet, will yet have to be elucidated - an involvement of the gut microbiome, by the way, is not impossible.
Bottom line: In the end, it may not even be important if non-celiac gluten sensitivity is a real or a social-psychological epidemic. If you are "infected" and avoiding gluten-containing foods and or non-fermentable short-chain carbohydrates helps you, do it! As long as you keep an eye on your micronutrient intake and don't live off ready-made processed gluten-free junk, it's probably not going to harm you - physiologically that is.
As far as to the psychological side effects are concerned, I am yet not sure, whether the constant (perceived) need to double check each and every product level is not going to drive one or another of the mostly already OCD-ridden anti-wheat-warriors to insanity.
Reference:  |
| It's not always easy to be "gluten-free", even for animals (Gulls Comic) |
- Biesiekierski, Jessica R., et al. "No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates." Gastroenterology 145.2 (2013): 320-328.
- Brouns, Fred JPH, Vincent J. van Buul, and Peter R. Shewry. "Does wheat make us fat and sick?." Journal of Cereal Science 58.2 (2013): 209-215.
- Catassi, Carlo, et al. "Non-Celiac Gluten sensitivity: the new frontier of gluten related disorders." Nutrients 5.10 (2013): 3839-3853.
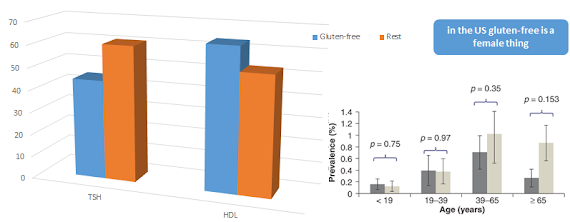
- DiGiacomo, Daniel V., et al. "Prevalence of gluten-free diet adherence among individuals without celiac disease in the USA: results from the Continuous National Health and Nutrition Examination Survey 2009-2010." Scandinavian journal of gastroenterology 48.8 (2013): 921-925.
- Golley, Sinéad et al. "Motivations for avoiding wheat consumption in Australia: results from a population survey." Public Health Nutrition (2014). First view available on CJO2014.
- Hallert, C., et al. "Quality of life of adult coeliac patients treated for 10 years." Scandinavian journal of gastroenterology 33.9 (1998): 933-938.
- Junker, Yvonne, et al. "Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4." The Journal of experimental medicine 209.13 (2012): 2395-2408.
- Long, K. H., et al. "The economics of coeliac disease: a population‐based study." Alimentary pharmacology & therapeutics 32.2 (2010): 261-269.
- Moore, Lauren Renée. "“But We’re Not Hypochondriacs”: The Changing Shape of Gluten-Free Dieting and the Contested Illness Experience." Social Science & Medicine (2014).
- Monsbakken, K. W., P. O. Vandvik, and P. G. Farup. "Perceived food intolerance in subjects with irritable bowel syndrome–etiology, prevalence and consequences." European journal of clinical nutrition 60.5 (2006): 667-672.
- Sollid, Ludvig M., and Bana Jabri. "Triggers and drivers of autoimmunity: lessons from coeliac disease." Nature Reviews Immunology 13.4 (2013): 294-302.
- Teufel, Martin, et al. "Psychological burden of food allergy." World Journal of Gastroenterology 13.25 (2007): 3456.