 |
| The power of GI calculations is limited and even with meals as simple as the one in the picture, the calculated glycemic index can be ~50% off! |
Use sugar alternatives if you want to improve your blood glucose!
"Before inclusion into the study, potential participants were briefed on all aspects of the experiment and were given the opportunity to ask questions. Following the securing of consent, a health assessment was performed which included anthropometric measurements and a health questionnaire (giving details of food allergies/intolerance, metabolic diseases, special dietary needs and smoking habits). Those who fulfilled all the inclusion criteria [body mass index 18.5–24.99 kg/m2; blood pressure (BP)—systolic BP between 110 and 120 mmHg and diastolic BP between 75 and 85 mmHg; age 21–50 years; fasting blood glucose, 4–6 mmol/L; not on prescription medication, non-smoking; no genetic or metabolic diseases) were enrolled into the study." (Sun. 2014)In addition, the amount of regular physical activity was quantified and subjects who were partaking in competitive sports and endurance events were excluded. Eventually, the scientists ended up with a group of normal-weight men and women at the age of 21–34 years.
 |
| Table 1: Composition of the test meals, ACHO = available carbohydrates. Nutritional data were obtained from the manufacturers (Sun. 2014). |
Ground nut oil? I guess most of you will know the oil that was used in the study at hand as "peanut oil" and it is - as you will probably know, as well - not exactly high in "holy" omega-3 fatty acids. Rather than that, peanut oil contains oleic acid (46.8% as olein), linoleic acid (33.4% as linolein), and palmitic acid (10.0% as palmitin), as well as small amounts of stearic acid, arachidic acid, arachidonic acid, behenic acid, lignoceric acid, but not a singly milligram of omega-3s.
The test or reference food was then given to consume within 15 min. Further blood samples for glucose and insulin analysis were taken for the subsequent 180 min (every 15 min in the first hour and every 30 min for the subsequent hours) - a procedure that yielded the following results.
The test or reference food was then given to consume within 15 min. Further blood samples for glucose and insulin analysis were taken for the subsequent 180 min (every 15 min in the first hour and every 30 min for the subsequent hours) - a procedure that yielded the following results.
 |
| Figure 1: Glucose levels expressed relative to the ingestion of 250g of glucose (Sun. 2014) |
Significant differences for the insulin response were observed for the white rice + chicken meal, where the insulin response was significantly higher compared to the white rice only (+22%), as well as the rice with + vegetable meal, where the insulin response was significantly lower compared to the white rice only condition (-16%).
The combination of foods determines the GI of the meal
Based on the classic equation that's usually used to determine the glycemic index of a meal (Hätönen. 2011), Sun et al. calculated the predicted glycemic of the five test meals and compared it to the actual glycemic index (GI) that was calculated based on the measured glucose and insulin response of the subjects.
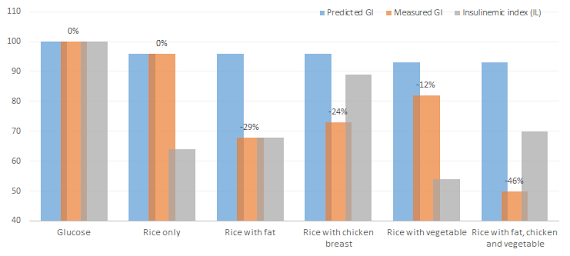 |
| Figure 2: Predicted and measured glycemic index as well as measured insulinemic index of the meals (Sun. 2014) |
 |
| Suggested Read: "Get Your Protein, Veggies & Fruits and Get Them Regularly: High(er) Meal Frequency (6 à Day) + High(er) Protein Diet Support Weight & Fat Loss on a Diet." | read more |
In contrast to what the "paleo hypothesis" and the notion that our ancestors would not have collected some berries or boiled some rice to have it alongside the chicken they just caught would say, the contemporary scientific evidence indicates that we are well equipped to handle complex meals, as long as they don't contain exorbitant amounts of fat and carbohydrates.
One thing we should not forget, though, is that the 50% discrepancy between the calculated and real glycemic index of the "complex" test meal (four ingredients is not exactly "complex", actually) suggests that one of the reasons that many of the previous studies failed to detect a meaningful association between the (obviously calculated) GI of an individuals diet and his / her cardiovascular or diabetes risk may be that the data the scientists used was similarly inaccurate as the predicted glycemic indices of the test meal in the study at hand | Comment on Facebook!
- Hätönen, Katja A., et al. "Protein and fat modify the glycaemic and insulinaemic responses to a mashed potato-based meal." British Journal of Nutrition 106.02 (2011): 248-253.
- Mah, Eunice, et al. "Postprandial hyperglycemia impairs vascular endothelial function in healthy men by inducing lipid peroxidation and increasing asymmetric dimethylarginine: arginine." The Journal of nutrition 141.11 (2011): 1961-1968.
- Sun, Lijuan, et al. "Effect of chicken, fat and vegetable on glycaemia and insulinaemia to a white rice-based meal in healthy adults." European journal of nutrition (2014): 1-8.
- Wolever, T. M. S. "Is glycaemic index (GI) a valid measure of carbohydrate quality&quest." European journal of clinical nutrition 67.5 (2013): 522-531.


