|
| Are the hormonal side effects of dairy and its cancerous consequences even worse than they're painted by the steadily growing anti-dairy lobby? |
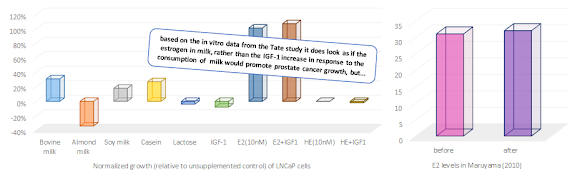
"[E]strogens in milk were absorbed, and gonadotropin secretion was suppressed, followed by a decrease in testosterone secretion"(Maryama. 2010) - Don't worry it looks worse than it is.
The above was the non-literal "bone of contention" Artur stumbled across on Pubmed. It's a literal quote from the conclusion of the previously mentioned Maryama paper in Pedriatrics Internatial and it is, as Artur rightly points out "a little concerting".I have to admit. At first sight the data in Figure 1 does look disconcerting, but if you knew something about the postprandial changes in testosterone concentration you wouldn't conduct a stupid study like this, where you measure the testosterone levels fasted, 1h before the ingestion of the meal and four times every hour after the intake. And if you did that, you would realize that you've just confirmed previous research, when you realize that, both, ...
- What about the kids: Maruyama et al. analyzed only the urinary hormone levels of the kids. This is at best evidence that some of the hormones are absorbed..., and excreted, again and thus not really relevant.the gradual decrease in serum LH and FSH concentration in six out of seven men that reached a nadir 60–120 min after the milk meal, as well as
- the decrease in serum testosterone concentrations which reached their minimal values ~ 120 min after the consumption of the milk in all subjects.
 |
| Figure 2: Macronutrient content (in g) of the test meals and corresponding postprandial reduction (% of baseline) of serum total tesosterone (Volek. 2001; Habito. 2001; Maruyama. 2010) |
- And what about the women: I have to apologize, but the researchers didn't find any abnormalities in the female study participants that would be of serious concern. I will still discuss the issue of possible increases in breast cancer risk due to a high dairy intake later in this article - promise!... the diarunal rhythm, i.e. the natural ups and downs in the course of the day allow for deviations of up to 38% (in some cases more; cf. Leymarie. 1974) in serum testosterone levels over a 24h period, and
- ... we usually don't drink milk that comes exclusively from pregnant cows, because the commercially available milk is a mix of milk from 100s if not 1000s of cows, so that the actual hormone levels in the raw milk mix are not going to be 10x higher than in pasture-fed cows who are milked only through the first three months of a new pregnancy (Shaw. 2007)
 |
| Figure 3: Estrone (E1) content in commercial milk, left; estrogen content in raw milk from non-pregant and pregnant cows in different tirmesters of the pregnancy (Farlow 2006; Malekinejad. 2009) |
Let's put these numbers into perspective:"The level in a liter of skim milk, for example, is approximately 667 times lower than the conjugated equine estrogens in low-dose Premarin (300 g) and 1389 times lower than standard dose Premarin (625 g), which is associated with breast cancer incidence in post-menopausal women after long-term exposure." (Farlow. 2009)
It goes without saying that this discrepancy between the assumed and the real amount of estrone in milk does not exactly increase the plausibility of the assumption that the epidemiological "evidence", i.e. cherry picked associations between nationwide dairy intakes, infertility and cancer rates Ganmaa et al. cite in the respective papers, warrants the conclusion that there was a causative link between the amount of milk and milk products you consume and your likelihood of developing reproductive disorders, prostate or breast cancer.Let's cherry pick some counter-evidence to the cherry-picked evidence!
If we simply assume that Ganmaa et al. and other researchers who subscribe to the "dairy is the devil" theory don't cite the existing counter-evidence. It should be easy to do some epidemiological cherry picking, ourselves, to support the safety of dairy, right? Right! And in the case of breast cancer, this is actually not really difficult:
-32% breast cancer risk in premenopausal women with one or more servings of low fat dairy per day (Shi. 2002)![]()
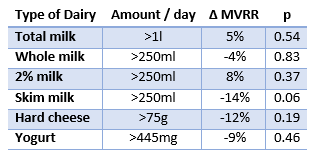
Table 1: Change in breast cancer Multivariable-adjusted relative risk with highest vs. lowest dairy consumption (Genkinger. 2013) - -19% breast cancer risk in postmenopausal women with two or more servings of dairy (McCullough. 2005)
- -86% breast cancer risk with highest dairy consumption in case control study in Iranian women (Bahadoran. 2013)
- -10% benign breast disease in young women with high milk intake at age 14 (Berkey. 2013)
in the Black Women’s Health Study by Jeanine M. Genkinger, Kepher H. Makambi, Julie R. Palmer, Lynn Rosenberg, and Lucile L. Adams-Campbell, who report that ...
"[...i]n this large prospective cohort of African-American women, null associations were observed for intakes of milk (total, whole, and 2 %), other specific types of dairy products, dietary calcium, and dietary vitamin D with breast cancer risk." (Genkinger. 2013)If you look at the p-values (remember: p > 0.05 ➲ not significant) in Table 1 it becomes even more obvious that we are dealing with a classic null-result here. If anything you could argue that there is a minimal protective effect with a high(er) intake of skim milk.
So dairy doesn't cause breast cancer... does it make men infertile, then?
 |
| Figure 4:Change in idiopathic asthenozoospermia w/ high vs. low intake of meat, sweets & dairy (Eslamian. 2012) |
These detrimental effects are yet by no means dairy exclusive (actually it should read "full-fat dairy exclusive", because most studies could not find negative effects for low fat dairy foods).
Mendiola et al. (2009), for example, observed a similar decline in sperm quality in men with a high processed meat intake and Eslamian et al. (2012) report that both, the total meat (+103%, p = 0.039) and sweets intake (+105%, p = 0.046), but not the amount of dairy the 72 asthenozoospermic men and 169 normo-zoospermic in Eslamian et al.'s case-control study consumed on a daily base were associated with a significantly higher risk of idiopathic asthenozoospermia (see Figure 4).
Saturated fat as common denominator? I know it's not popular, but processed meat and high fat dairy have a significant amount of saturated fat, which has been implicated as another correlate of reductions in sperm quality in a whole host of studies. Most recently Jensen et al. observed 38% (95% CI: 0.1%, 61%) lower sperm concentration and a 41% (95% CI: 4%, 64%) lower total sperm count in 701 young Danish men with high vs. low saturated fat intake (Jensen. 2013). In view of the less significant, but more pronounced associaton of asthenozoospermia with high sweet intakes, Eslamian et al. report in their 2012 paper, I would yet suspect that overeating and not fats or carbs are the real problem, here.
If finding evidence that the dairy ↔ infertility issue isn't an issue at all was hard, doing the same for epidemiologically established link between high(er) dairy intakes and prostate cancer is ... not virtually impossible, but significantly harder.Last but not least, the prostate cancer issue
There is in fact a whole host of studies a litigator could chose from, if he decided to sue the dairy industry and I have to admit that I wouldn't want to wear the gown that indicates that it's up to me to decide whether evidence such as, the...
- 3.2x increase in advanced prostate cancer risk in men who consumed dairy products on a daily basis as adolescents, Torfadottir et al. observed in 8,894 men who were born between 1907 and 1935 in Iceland (Torfadottir. 2012),
- 2.2x increase in prostate cancer risk in US men who consumed 21 or more servings of dairy products per week vs. those who consumed only 5 servings/week (Tseng. 2005)
- 1.68x higher risk of prostate cancer risk researchers calculated in a meta-analysis of case-control studies published between 1984 and 2003 (Qin. 2007)
Let's not forget the changes in estrone and progesterone
We would thus be back to square one and our initial assumption that all that cannot be so bad, as it may have looked at first sight, if we it was not for two significant changes Maryama et al. observed in their experiment, we have hitherto ignored: The +26% and +14% increases in estrone (E1) and progesterone levels, respectively.
We have touched on estrone already. It is one of several natural estrogens and is abundant primarily during pregnancy (which explains why it's high in the milk of pregnant cows) and while the Wikipedia entry on estrone says that it was "known to cause anorexia, nausea, vomiting, and erectile dysfunction" the reference the author provides is an info-document from the United States Department of Labor.
And what about female libido? I did not forget you, ladies. The thing is with the high amount of estrone and progesterone you already have in your body, the minimal amount you may be getting from milk is probably not going to have any effects on your libido.
If you try to find corresponding evidence in peer reviewed magazines, on the other hand, you come up with a report by Jerzy Terter that was published in the British Medical Journal in October 1972 and says that estrone and estrone & testosterone have been used successfully to treat, not induce erectile dysfunction (Terter. 1972). Similar restorative effects have been reported for a combination of estrogen and progesterone, which was more effective in increasing coital frequency in male castrats than testosterone (Davidson. 1983)Fine, libido / erectile performance shouldn't be an issue, but what about cancer?
Even if the small quantities of estrone and progesterone don't mess with your libido, this does not mean that they cannot (in the very long term) increase your risk of prostate or breast cancer, right? Since we've wantonly neglected the ladies in the previous paragraphs we'll start out with the breast cancer issue and the question: "Do progesterone or estrone increase your breast or endometrial cancer risk?"
- Progesterone and breast, endometrial cancer & co: Despite the fact that studies from the 1980s show that progesterone deficiency increases the risk of developing breast cancer before menopause by more than 400% (Cowan. 1981) and in spite of recent evidence that progesterone enhances the anti-cancer effects of calcitriol (active vitamin D; cf. Lee. 2013), the rumor that progesterone / protestin based oral contraceptives would promote the growth of all sorts of cancer is tenacious.Possible health problems due to low progesterone (in pre- menopausal women): Low blood sugar, foggy thinking, uterine fibroids, decreased sweating, fibrocystic breasts, low blood pressure, tender breasts, infertility, chemical sensitivity, cold body temperature (ordered from lowest to highest incidence).Evidence from the early 1980 would in fact support the progesterone cancer association (Pike. 1982). If you know something about the hormonal content of the "early pill", it's no wonder that the observations Pike et al. made in the 1980s stand in contrast to the results of more recent studies on associations between oral contraceptives and breast or other forms of cancer. Studies like the one by Marchbanks et al., for example. In the corresponding paper, the researchers report ZERO increase in breast cancer risk for current oral contraceptive users and a 10% reduced breast cancer risk for those of the 4575 women with breast cancer and 4682 controls who had previously used them (Marchbanks. 2002).
It goes without saying that there are also more recent studies suggesting risk increases with oral contraceptive for various forms of cancer. The total amount, but also the type of progesteron (bovine vs. articial, sometimes much stronger progestins) do make it very unlikely that milk will promote breast cancer growth... incidentally, the previously discussed in vitro study by Tate et al. (2011) confirms that. In the said study milk may have promoted the growth of the prostate cancer cells, the breast cancer cells, the researchers tested as well, did yet not respond to be being bathed in a Petri dish full of bovine milk. Much contrary to soymilk, by the way, which promoted the growth of Tate et al.'s breast cancer cells magnificently. - Estrone and breast, endometrial cancer & co: In view of the fact that estrone is capable of binding to the estrogen receptor on breast cancer cells and considering the fact that Toniolo et al. observed in a 1995 prospective study of endogenous estrogens and breast cancer in postmenopausal women that women with estrone levels between 12.3pg/ml and 20.9pg/ml had a 3.7x elevated breast cancer risk compared to those with estrone levels of 8pg/ml or less (Toniolo. 1995). Similar results were reported only recently by Farhat et al. (2013) for premenopausal women whose breast cancer risk is 3x elevated with estrone levels of 50.39-151.39pg/ml vs. 9.05-27.86 (Farhat. 2013)
In view of the fact that I could not find a definitive number for the oral bioavailability of estrone, I had to use the C-max (max. concentration) values from a 1990 study by Aedo et al. to estimate whether the maximal amount of estrone you can find in cow's milk, i.e. ~100pg/ml could elevate a woman's E2 levels to an extend that would put her into a higher breast cancer risk category.
Why don't we use the values from the Maruyama study? I am pretty certain that it would be a bad idea to extrapolate estrogen / estrone related data from a study, where the corresponding levels were measured only in men to women. Moroever, even if we did that, we would still be faced with the problem that the peak values Maruyama et al. measured are probably irrelevant in terms of cancerous growth, which thrives in a milieu with constantly elevated estrone levels and is unlikely to grow in response to intermediate peaks that last for less than an hour.
- In the said study the area under the estrone in response to the ingestion of 2.5mg of estrone-sulfate was 5.32 ng/ml per hour.
In simple (from a science point of view questionable) analogy, one liter of bovine milk from a pregnant cow in the third trimester (=highest estrone content; ca. 100pg/ml) would thus create an AUC of only 0.2pg/ml per hour. If you look at the data in Table 2 it should be obvious that this is not going to take a women from Q1 with E2 levels of 9.05–27.86pg/ml to Q3 (36.79–50.38 pg/ml) the first quartile, where the risk increase becomes statistically significant.![]()
Table 2: Association of estrone levels with invasive breast cancer risk (Farhat. 2013)
Honestly, I would not rely on hilariously inaccurate calculations like this, if the available epidemiological evidence I discussed before would not indicate that the consumption of bovine milk does not increase the risk of developing breast cancer, although the number of potential mechanisms, e.g. high estrogen, high estrone, high progesterone, overactivation of mTOR and IGF-1, are endless. Moreover, similar protective effects have been observed for ovarian cancer with (interestingly, they mostly ascribed to dairy calcium, though)- skim or low fat milk - 13-15% reduction, when consumed regularly
- hard cheese - up to 32% reduction when consumed 2-7 days per week
- cottage and ricoatte chesse - up to 24% when consumed 2-7 days per week
- Progesterone and prostate cancer in men: With a normal range of 0.27 – 0.9 ng/ml the progesterone levels in the Maruyama study, i.e. 0.75ng/ml are still well within the normal range, for men. This and the mere facts that
- there is a host of research that confirms that the majority prostate cancer cells don't even have a progesterone receptor (Hobisch. 1997; Gregory),
- the progesterone receptors in prostate stromal fibroblasts and smooth muscle cells, suppress prostate stromal cell proliferation (Yu. 2013), and
- studies like Umekita (1996) suggest that medroxy progesterone acetate inhibits the growth of LNCaP prostate cancer cells in the Petri dish (Umekita. 1996)
- Estrone and prostate cancer risk in men: As far as the estrone levels Maruyama et al. measured in their 2010 study are concerned it is very difficult to tell, whether or not the 26% increase in E2 levels is or isn't a problem.
The estrone values in the Maruyama study are unrealistic. With a normal range of <68pg/ml the subjects in the Maruyama study would have elevated E1 levels to begin with, if the measurement was correct.
- According to a study by Hsing & Comstock, prostate cancer patients have lower estrone : testosterone ratios than healthy controls (Hsing. 1993). In their 1988 paper Nomura et al. had already reported that prostate cancer patients have 26.7% lower estrone levels than healthy controls (Nomura. 1988); an observation that confirms the results of a previous analysis of estrone levels in US and Nigerian men by Ahluwalia from 1981 (Ahluwalia. 1981). In all but the Nigerians, the differences were yet not significant, which is why I would hesitate to use these observations to support the hypothesis that the changes in estrone and testosterone Maruyama et al. observed may actually protect against breast cancer.
In spite of a study by Giton et al. (2008) that implicates estrone sulfate, which happens to be elevated in the presence of high estradiol levels (probably the real culprit here) as a marker of tumor aggressiveness, it would thus appear unwarranted to worry about the estrone increase in the Maruyama study, if we focus on a 26% from a midrange estrone value (see red box above for an explanation of why I don't use the exact serum values from the study) values are even accurate.
| A high dairy intake... | |
| lowers testosterone | ✘ |
| impairs libido | ✘ |
| impairs fertility | ✘ |
| disturbs regular menses | ✘ |
| promotes prostate cancer | ✔ |
| promotes breast cancer | ✘ |
| promotes any type of cancer | ❓ |
- ✘ - indicates low-to-no evidence, while
- ❓ - tells you that things are not certain, yet and
- ✔ - marks a potential reason to stay away from dairy
- Aedo, A. R., Landgren, B. M., & Diczfalusy, E. (1990). Pharmacokinetics and biotransformation of orally administered oestrone sulphate and oestradiol valerate in post-menopausal women. Maturitas, 12(4), 333-343.
- Afeiche, M., Williams, P. L., Mendiola, J., Gaskins, A. J., Jørgensen, N., Swan, S. H., & Chavarro, J. E. (2013). Dairy food intake in relation to semen quality and reproductive hormone levels among physically active young men. Human Reproduction.
- Ahluwalia, B., Jackson, M. A., Jones, G. W., Williams, A. O., Rao, M. S., & Rajguru, S. (1981). Blood hormone profiles in prostate cancer patients in high‐risk and low‐risk populations. Cancer, 48(10), 2267-2273.
- Bahadoran, Z., Karimi, Z., Houshiar-rad, A., Mirzayi, H. R., & Rashidkhani, B. (2013). Is Dairy Intake Associated to Breast Cancer? A Case Control Study of Iranian Women. Nutrition and cancer, 65(8), 1164-1170.
- Berkey, C. S., Willett, W. C., Tamimi, R. M., Rosner, B., Frazier, A. L., & Colditz, G. A. (2013). Dairy Intakes in Older Girls and Risk of Benign Breast Disease in Young Women. Cancer Epidemiology Biomarkers & Prevention, 22(4), 670-674.
- Bonkhoff, H., Fixemer, T., Hunsicker, I., & Remberger, K. (2001). Progesterone receptor expression in human prostate cancer: correlation with tumor progression. The Prostate, 48(4), 285-291.
- Chagas, C. E., Rogero, M. M., & Martini, L. A. (2012). Evaluating the links between intake of milk/dairy products and cancer. Nutrition reviews, 70(5), 294-300.
- Cordain, H. D. The Adverse Effects of Milk-by Loren Cordain & Pedro Bastos.
- Cowan, L. D., Gordis, L., TONASCIA, J. A., & Jones, G. S. (1981). Breast cancer incidence in women with a history of progesterone deficiency. American journal of epidemiology, 114(2), 209-217.
- Davidson, J. M., Camargo, C., Smith, E. R., & Kwan, M. (1983). Maintenance of sexual function in a castrated man treated with ovarian steroids. Archives of Sexual Behavior, 12(3), 263-274.
- Eslamian, G., Amirjannati, N., Rashidkhani, B., Sadeghi, M. R., & Hekmatdoost, A. (2012). Intake of food groups and idiopathic asthenozoospermia: a case–control study. Human Reproduction, 27(11), 3328-3336.
- Farhat, G. N., Parimi, N., Chlebowski, R. T., Manson, J. E., Anderson, G., Huang, A. J., ... & Cummings, S. R. (2013). Sex Hormone levels and risk of Breast cancer With estrogen Plus Progestin. Journal of the National Cancer Institute, 105(19), 1496-1503.
- Farlow, D. W., Xu, X., & Veenstra, T. D. (2009). Quantitative measurement of endogenous estrogen metabolites, risk-factors for development of breast cancer, in commercial milk products by LC–MS/MS. Journal of Chromatography B, 877(13), 1327-1334.
- Ganmaa, D., Wang, P. Y., Qin, L. Q., Hoshi, K., & Sato, A. (2001). Is milk responsible for male reproductive disorders?. Medical hypotheses, 57(4), 510-514.
- Ganmaa, D., Li, X. M., Wang, J., Qin, L. Q., Wang, P. Y., & Sato, A. (2002). Incidence and mortality of testicular and prostatic cancers in relation to world dietary practices. International journal of cancer, 98(2), 262-267.
- Ganmaa, D., & Sato, A. (2005). The possible role of female sex hormones in milk from pregnant cows in the development of breast, ovarian and corpus uteri cancers. Medical hypotheses, 65(6), 1028-1037.
- Giton, F., de la Taille, A., Allory, Y., Galons, H., Vacherot, F., Soyeux, P., ... & Fiet, J. (2008). Estrone sulfate (E1 S), a prognosis marker for tumor aggressiveness in prostate cancer (PCa). The Journal of steroid biochemistry and molecular biology, 109(1), 158-167.
- Genkinger, J. M., Makambi, K. H., Palmer, J. R., Rosenberg, L., & Adams-Campbell, L. L. (2013). Consumption of dairy and meat in relation to breast cancer risk in the Black Women’s Health Study. Cancer Causes & Control, 1-10.
- Gregory, C. W., He, B., Johnson, R. T., Ford, O. H., Mohler, J. L., French, F. S., & Wilson, E. M. (2001). A mechanism for androgen receptor-mediated prostate cancer recurrence after androgen deprivation therapy. Cancer research, 61(11), 4315-4319.
- Habito, R. C., & Ball, M. J. (2001). Postprandial changes in sex hormones after meals of different composition. Metabolism, 50(5), 505-511.
- Hsing, A. W., & Comstock, G. W. (1993). Serological precursors of cancer: serum hormones and risk of subsequent prostate cancer. Cancer Epidemiology Biomarkers & Prevention, 2(1), 27-32.
- Hobisch, A., Hittmair, A., Daxenbichler, G., Wille, S., Radmayr, C., Hobisch‐Hagen, P., ... & Culig, Z. (1997). Metastatic lesions from prostate cancer do not express oestrogen and progesterone receptors. The Journal of pathology, 182(3), 356-361.
- Jensen, T. K., Heitmann, B. L., Jensen, M. B., Halldorsson, T. I., Andersson, A. M., Skakkebæk, N. E., ... & Jørgensen, N. (2013). High dietary intake of saturated fat is associated with reduced semen quality among 701 young Danish men from the general population. The American journal of clinical nutrition, 97(2), 411-418.
- Jouan, P. N., Pouliot, Y., Gauthier, S. F., & Laforest, J. P. (2006). Hormones in bovine milk and milk products: a survey. International Dairy Journal, 16(11), 1408-1414.
- Lee, L. R., Teng, P. N., Nguyen, H., Hood, B. L., Kavandi, L., Wang, G., ... & Syed, V. (2013). Progesterone Enhances Calcitriol Antitumor Activity by Upregulating Vitamin D Receptor Expression and Promoting Apoptosis in Endometrial Cancer Cells. Cancer Prevention Research.
- Malekinejad, H., Scherpenisse, P., & Bergwerff, A. A. (2006). Naturally occurring estrogens in processed milk and in raw milk (from gestated cows). Journal of agricultural and food chemistry, 54(26), 9785-9791.
- Marchbanks, P. A., McDonald, J. A., Wilson, H. G., Folger, S. G., Mandel, M. G., Daling, J. R., ... & Weiss, L. K. (2002). Oral contraceptives and the risk of breast cancer. New England Journal of Medicine, 346(26), 2025-2032.
- Maruyama, K., Oshima, T., & Ohyama, K. (2010). Exposure to exogenous estrogen through intake of commercial milk produced from pregnant cows. Pediatrics International, 52(1), 33-38.
- McCullough, M. L., Rodriguez, C., Diver, W. R., Feigelson, H. S., Stevens, V. L., Thun, M. J., & Calle, E. E. (2005). Dairy, calcium, and vitamin D intake and postmenopausal breast cancer risk in the Cancer Prevention Study II Nutrition Cohort. Cancer Epidemiology Biomarkers & Prevention, 14(12), 2898-2904.
- Mendiola, J., Torres-Cantero, A. M., Moreno-Grau, J. M., Ten, J., Roca, M., Moreno-Grau, S., & Bernabeu, R. (2009). Food intake and its relationship with semen quality: a case-control study. Fertility and sterility, 91(3), 812-818.
- Merritt, M. A., Cramer, D. W., Vitonis, A. F., Titus, L. J., & Terry, K. L. (2013). Dairy foods and nutrients in relation to risk of ovarian cancer and major histological subtypes. International Journal of Cancer, 132(5), 1114-1124.
- Nomura, A., Heilbrun, L. K., Stemmermann, G. N., & Judd, H. L. (1988). Prediagnostic serum hormones and the risk of prostate cancer. Cancer research, 48(12), 3515-3517.
- Parodi, P. W. (2012). Impact of cows’ milk estrogen on cancer risk. International Dairy Journal, 22(1), 3-14.
- Park, Y., Mitrou, P. N., Kipnis, V., Hollenbeck, A., Schatzkin, A., & Leitzmann, M. F. (2007). Calcium, Dairy Foods, and Risk of Incident and Fatal Prostate Cancer The NIH-AARP Diet and Health Study. American journal of epidemiology, 166(11), 1270-1279.
- Pike, M. C., Krailo, M. D., Henderson, B. E., Duke, A., & Roy, S. (1983). Breast cancer in young women and use of oral contraceptives: possible modifying effect of formulation and age at use. The Lancet, 322(8356), 926-929.
- Qin, L., Xu, J., Wang, P., Tong, J., & Hoshi, K. (2007). Milk consumption is a risk factor for prostate cancer in Western countries: evidence from cohort studies. Asia Pacific journal of clinical nutrition, 16(3), 467.
- Shaw, S. (2007) Modern Milk. Discussing research by Ganmaa Davaasambuu. Harvard Magazine. May-June.
- Shin, M. H., Holmes, M. D., Hankinson, S. E., Wu, K., Colditz, G. A., & Willett, W. C. (2002). Intake of dairy products, calcium, and vitamin D and risk of breast cancer. Journal of the National Cancer Institute, 94(17), 1301-1310.
- Tate, P. L., Bibb, R., & Larcom, L. L. (2011). Milk stimulates growth of prostate cancer cells in culture. Nutrition and cancer, 63(8), 1361-1366.
- Teter, J. (1972). Treatment of endocrine impotence. British medical journal, 4(5832), 114.
- Toniolo, P. G., Levitz, M., Zeleniuch-Jacquotte, A., Banerjee, S., Koenig, K. L., Shore, R. E., ... & Pasternack, B. S. (1995). A prospective study of endogenous estrogens and breast cancer in postmenopausal women. Journal of the National Cancer Institute, 87(3), 190-197.
- Torfadottir, J. E., Steingrimsdottir, L., Mucci, L., Aspelund, T., Kasperzyk, J. L., Olafsson, O., ... & Valdimarsdottir, U. A. (2012). Milk intake in early life and risk of advanced prostate cancer. American journal of epidemiology, 175(2), 144-153.
- Tseng, M., Breslow, R. A., Graubard, B. I., & Ziegler, R. G. (2005). Dairy, calcium, and vitamin D intakes and prostate cancer risk in the National Health and Nutrition Examination Epidemiologic Follow-up Study cohort. The American journal of clinical nutrition, 81(5), 1147-1154.
- Umekita, Y., Hiipakka, R. A., Kokontis, J. M., & Liao, S. (1996). Human prostate tumor growth in athymic mice: inhibition by androgens and stimulation by finasteride. Proceedings of the National Academy of Sciences, 93(21), 11802-11807.
- Volek, J. S., Love, D. M., Avery, N. G., Sharman, M. J., & Kraemer, W. J. (2001). Effects of a high-fat diet on postabsorptive and postprandial testosterone responses to a fat-rich meal. Metabolism, 50(11), 1351-1355.